The IVF Process
Overview of The IVF Process
In Vitro Fertilization (IVF) is the most effective fertility treatment available, offering the shortest time to pregnancy compared with other fertility options or natural conception.
IVF is a complex treatment, and the number of steps involved can make it seem overwhelming at first. The process involves numerous carefully coordinated tasks performed by patients, doctors, nurses, embryologists, and laboratory staff.
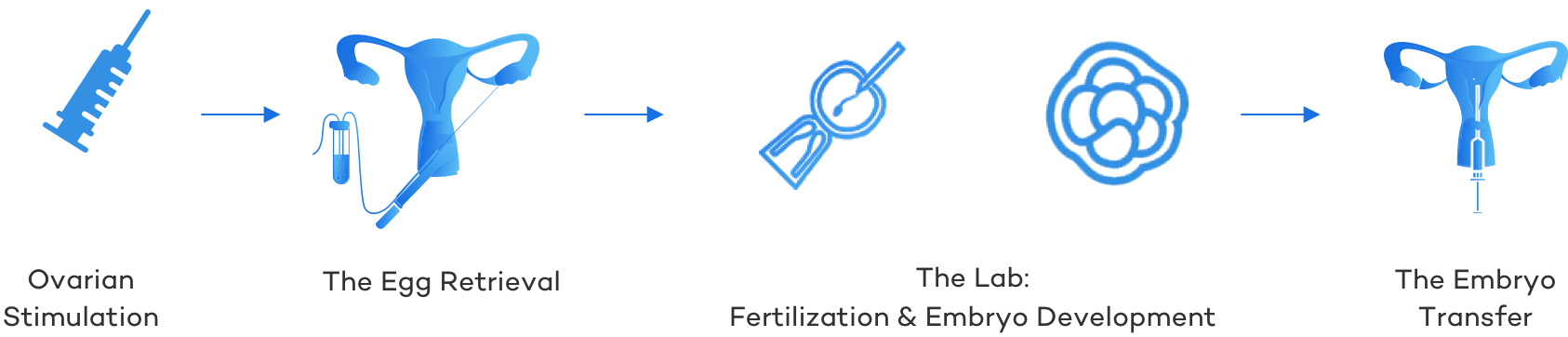
While it’s true that IVF requires precision and teamwork to be successful, the journey can be understood more easily when broken down into four main stages:
- Ovarian Stimulation: Hormone based medications are taken to improve the number and quality of eggs.
- The Egg Retrieval: A relatively mild surgical procedure under light anesthesia to remove the eggs from the ovaries.
- The IVF/Embryology Laboratory: Where both fertilization of the eggs with sperm takes place and early embryonic development.
- The Embryo Transfer: An embryo is loaded into a flexible catheter and deposited into the woman’s uterus.
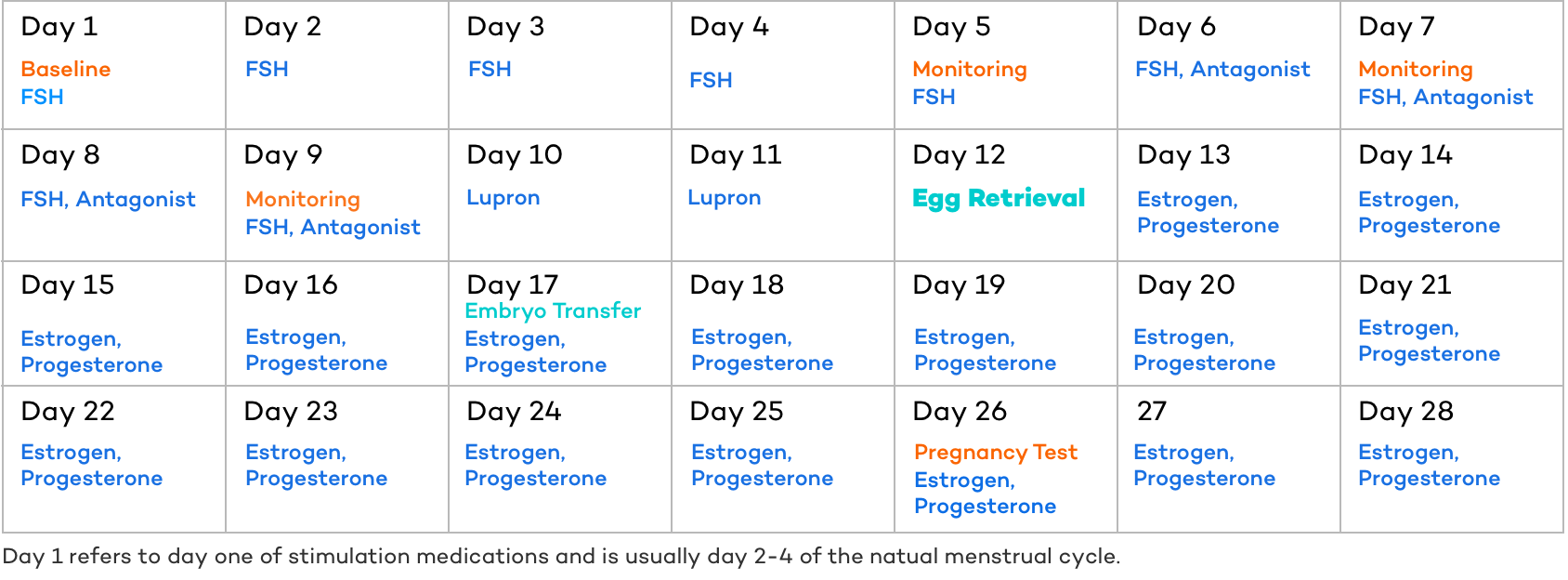
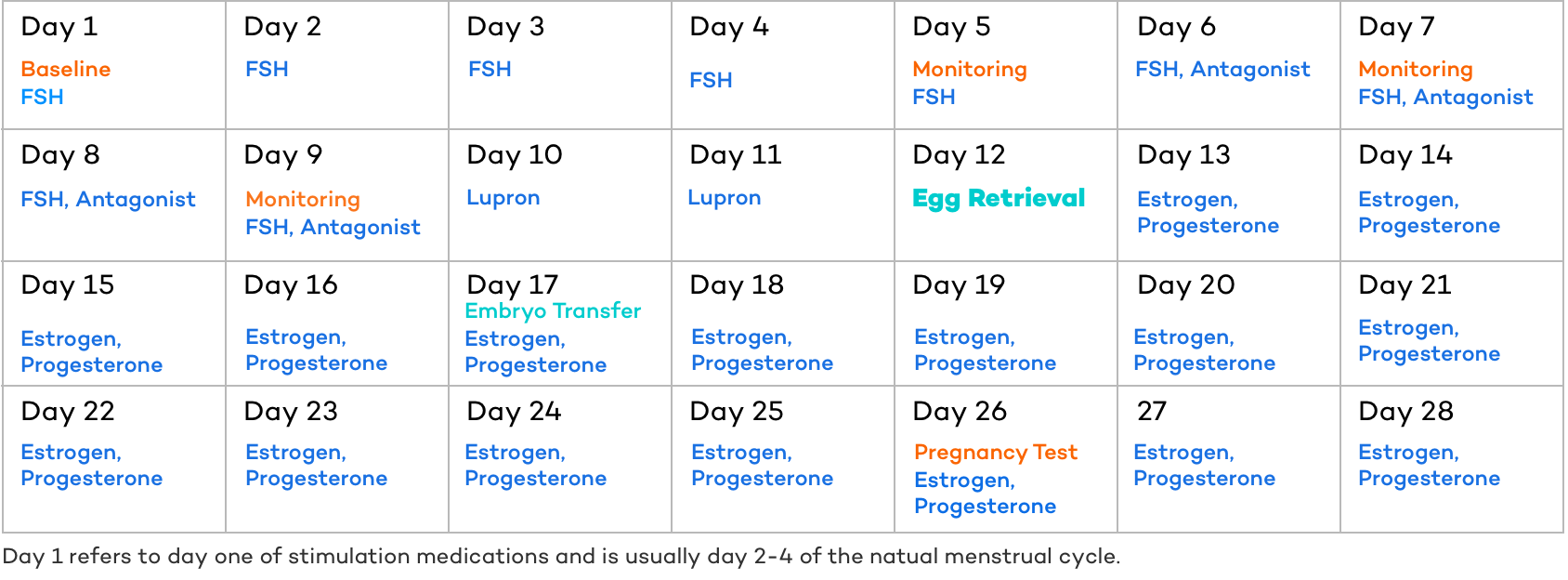
The timeline or exact day for each event during the IVF treatment process is highly variable from patient to patient and cycle to cycle, but in general looks something similar to the calendar below.
If one element shifts, everything following that event shifts in a similar manner. For example, if the follicles are not developing as rapidly as “expected,” the trigger shot (Lupron in the example below) would be delayed, which would then push back the egg retrieval, embryo transfer, and pregnancy test.
Now that we have a high-level overview of the in vitro fertilization process – let’s take a deep dive into each of the four major steps.
Step 1 of the IVF Process: Ovarian Stimulation
Ovarian stimulation is the phase of the In Vitro Fertilization process in which medications (FSH and sometimes LH) are taken so that the woman produces many mature eggs – as opposed to the one or two eggs a woman normally produces. Although there are variations of the IVF treatment like natural IVF, which does not use medications, and Mini IVF, which use different or lower doses of medications with the intention of producing only a few mature eggs, most experts agree that a good simulation is critical to the in vitro fertilization process.
Why exactly is ovarian stimulation so important?
The purpose of ovarian stimulation is straightforward: to increase the number of eggs available.
At every stage of IVF, there is natural attrition. An egg cannot be retrieved from every follicle, not every retrieved egg is mature, not every mature egg fertilizes successfully, not every fertilized egg develops into a healthy embryo, not every transferred embryo results in pregnancy, and not every pregnancy leads to a live birth.
By starting with more eggs, the chances of having viable embryos, and ultimately achieving a live birth, are much higher. Ovarian stimulation is what makes that possible.
As you might expect, numerous studies , show that the odds of a live birth rise drastically as the number of eggs retrieved goes up.
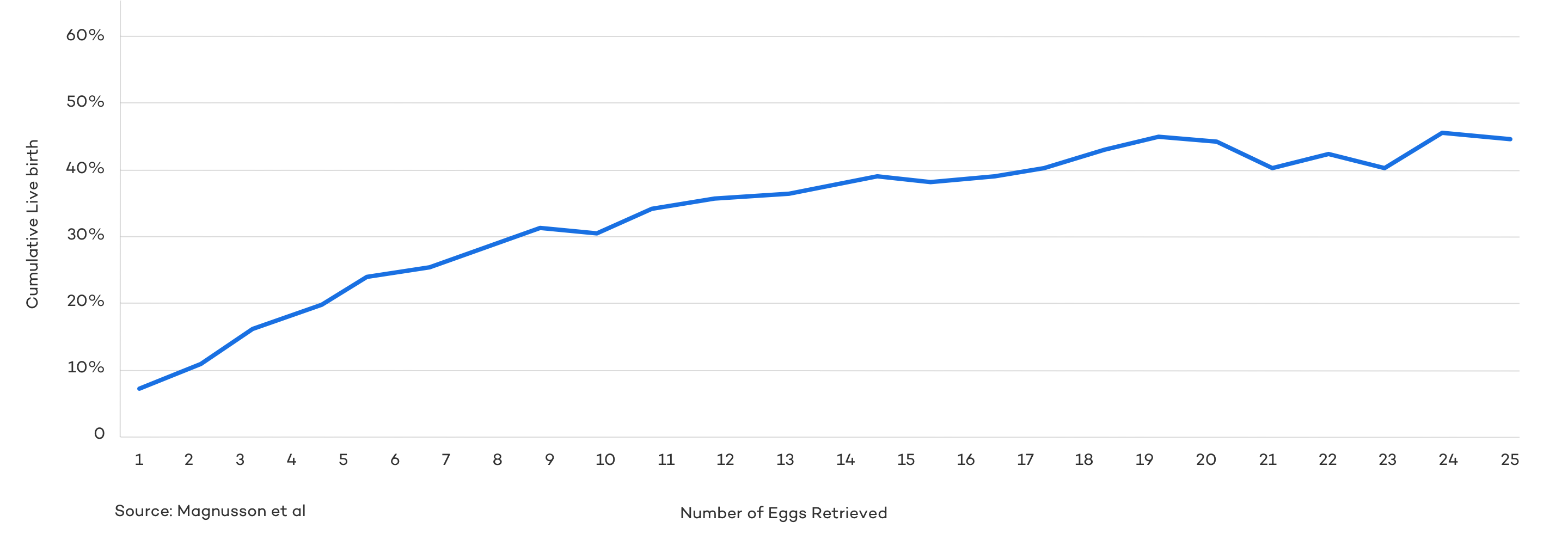
As you can see, the chances of success rise steadily as the number of eggs retrieved increases, until reaching a range of about 15–20. Beyond this point, additional eggs don’t significantly boost the odds of a live birth and may even raise the risk of complications.
The medications used to stimulate egg growth, particularly high doses of FSH, can sometimes cause ovarian hyperstimulation syndrome (OHSS).
While mild OHSS is relatively common, moderate to severe cases—occurring in about 1–5% of IVF cycles—can be serious and may require hospitalization. The risk is higher in younger women, those with elevated AMH levels, and women with polycystic ovary syndrome (PCOS).
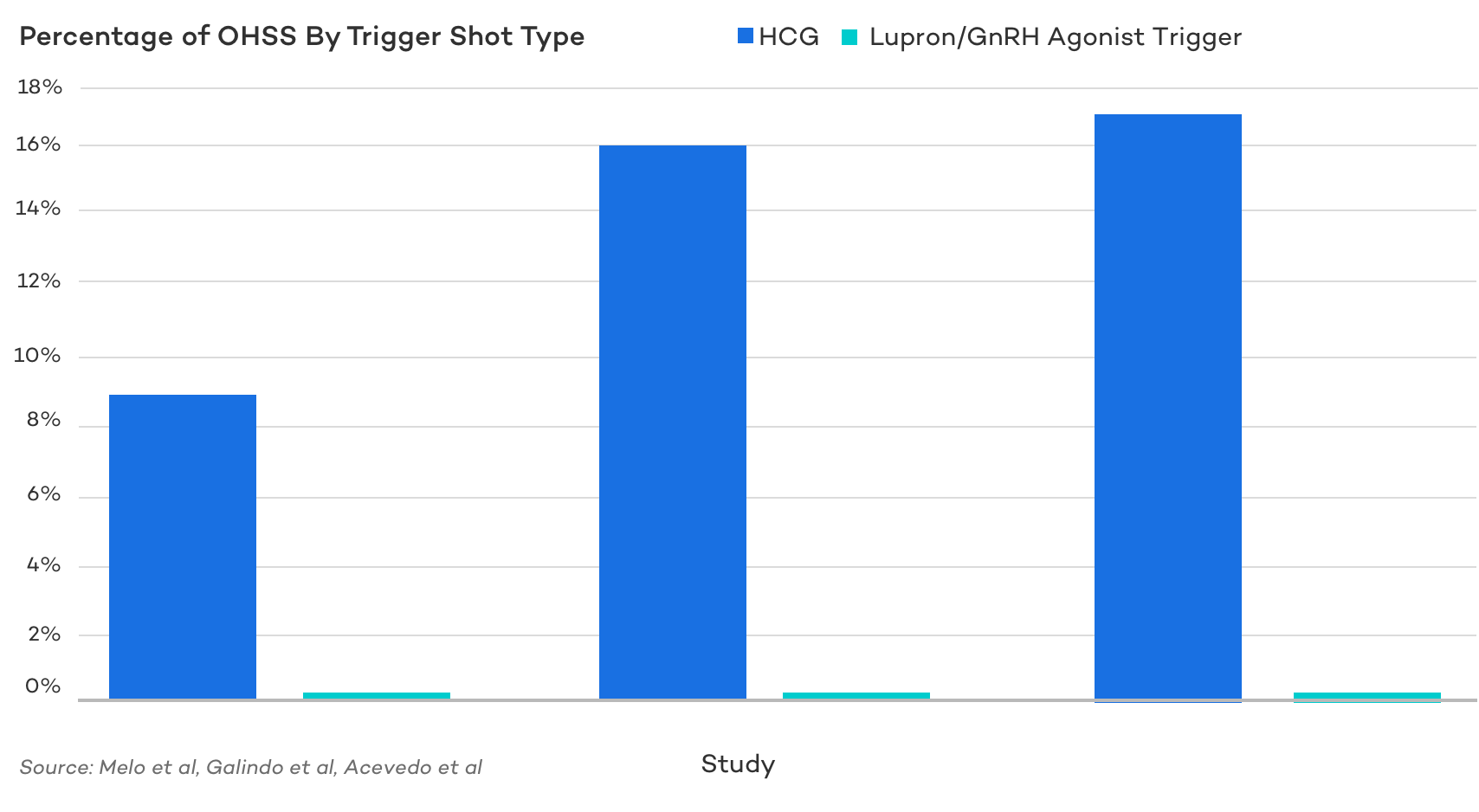
Fortunately, through close monitoring, appropriate dosing, and the proper choice of trigger medications, serious hyperstimulation can be largely avoided. In fact, simply following an antagonist protocol rather than an agonist protocol reduces the odds of hyperstimulation form 12 to 2.7% percent . And using a Lupron/GnRH trigger rather than an hCG trigger reduces the odds seemingly virtually .
Because of this, it’s important to work closely with your fertility doctor and nursing staff to develop an appropriate protocol to optimize the odds of success while mitigating risk.
Ovarian Stimulation Timeline:
Ovarian stimulation typically starts on day 2-4 of a woman’s natural menstrual cycle and usually lasts for 10-12 days.
Most often, a patient will be instructed to call the clinic on day one of their menstrual cycle to inform the clinic that their cycle has begun, and they would like to start a treatment cycle. They will then be scheduled to come into the office on cycle day 2-4 for a “baseline” office visit to establish “baseline” measures of follicular size, uterine lining, and hormone levels and to receive instructions on starting the treatment cycle.
It’s important to note that days of an IVF cycle can be confusing as some may refer to day one as the first day of the menstrual cycle where others refer to day one as the first day of FSH injections (and thus day one of treatment would be day 2-4 of the menstrual cycle). For purposes of this article, we will always use day 1 to mean the first day of IVF stimulation medications.
During the ovarian stimulation phase of the IVF process, FSH is taken for approximately 8-12 days. An antagonist medication that prevents ovulation is usually started in addition to FSH around day 5 or 6 (but the true day it is started is determined by the size of the follicles (usually 13mm) and/or your Estrogen levels). A trigger medication is then taken for one or two days, typically around day 10-14 to assist in the final maturation of the eggs.
Here is an example of a day by day look at ovarian stimulation:
- Day 1: The patient will come into the office for the baseline ultrasound and bloodwork testing. FSH injections are started the same day.
- Day 2: The patient takes FSH.
- Day 3: The patient takes FSH.
- Day 4: The patient takes FSH.
- Day 5: The patient takes FSH. The patient comes to the office for a monitoring appointment.
- Day 6: The patient takes FSH AND starts taking an antagonist medication (like Cetrorelix [Cetrotide] or Antagon [Ganirelix]), which prevent ovulation from happening.
- Day 7: The patient takes FSH AND antagonist. The patient comes to the office for a monitoring appointment.
- Day 8: The patient takes FSH AND antagonist
- Day 9: The patient takes FSH AND antagonist. The patient comes to the office for a monitoring appointment.
- Day 10: The patient stops taking takes FSH, and the antagonist AND takes a trigger medication (Leuprolide Acetate [Lupron] and/or hCG [Pregnyl, Profasi, Novarel, Ovidrel]) which induces the final maturation of the eggs and ovulation (of course the egg retrieval will take place before the eggs are truly ovulated. The egg retrieval will be scheduled 35 hours after this trigger injection.
- Day 11: If the patient only takes hCG as the trigger, they will usually not take any medications this day (unless using an immune protocol on top of the standard IVF protocol). If the patient is using Lupron only or Lupron and hCG as the trigger, the patient will administer another injection of Lupron (no hCG).
The Egg Retrieval: Step 2 of the IVF Process
The egg retrieval will be 35 hours after the trigger shot. You will be given a specific time to arrive at the office at which the retrieval is taking place. The egg retrieval is an ambulatory procedure that requires a sterile environment and mild anesthesia. For that reason, you will need to have arrangements made for someone to drive you home or to your hotel. Often this is a partner, friend, or loved one, but can certainly be a Medicab service if alone. Your partner or loved one will not be allowed in the room.
Preparing for The Egg Retrieval
You will likely be instructed to follow a number of precautions and instructions when preparing for the egg retrieval. For example:
The night and morning before the retrieval
- Do not to eat or drink after midnight the night before the egg retrieval
- Ensure you have someone to bring you to the office and drive you home
- Make a list of all the medications you have at home; the nurses will tell you when to start everything
- Wear comfortable clothing to the office
- If you are traveling from far away, you may want to bring a pillow and blanket for the car.
- If it takes you less than four hours to get to the office, you may collect your semen sample at home. Keep it warm by placing the cup inside your shirt.
When you arrive
- You will be greeted by the front desk staff. The front office staff will check you in and review all consents/financial contracts.
- It is helpful to arrive a little early so any remaining paperwork can be finished.
- If you have brought your semen sample with you, the front desk staff will take the container from you.
When your name is called
- You will be greeted by a nurse who will introduce themself.
- The nurse will escort you to your egg retrieval room while, if applicable, your partner will be escorted to our collection room to provide his semen sample.
- You will undress and change into a gown and robe.
- You will meet with the OR nurse and be prepped for the surgery. This includes bloodwork and attaching monitors to watch blood oxygen levels and heart rate band blood pressure as well as an IV line. Monitors will be used to watch your blood pressure, pulse, and temperature.
- You will also meet with the physician performing your procedure, the Anesthesiologist, and your Embryologist.
- *Sperm collection for IVF is usually provided the morning of the egg retrieval, but can also be collected in advance, prepared, frozen, and then later thawed the morning of the egg retrieval. If the sperm is being provided by a male partner, it is most often collected through ejaculation into a sterile cup either in our office or at home. If necessary, sperm can be collected using more advanced sperm retrieval procedures like PESA or TESA. If your male partner is providing the semen sample, we recommend abstaining from sexual intercourse or any means of ejaculation for at least two days but no longer than five days. If the sperm is being provided by a donor, we will need the sperm in our office at the beginning of your cycle.*
When its time for your procedure
- You will receive medications through the IV to make you sleepy and comfortable throughout your procedure
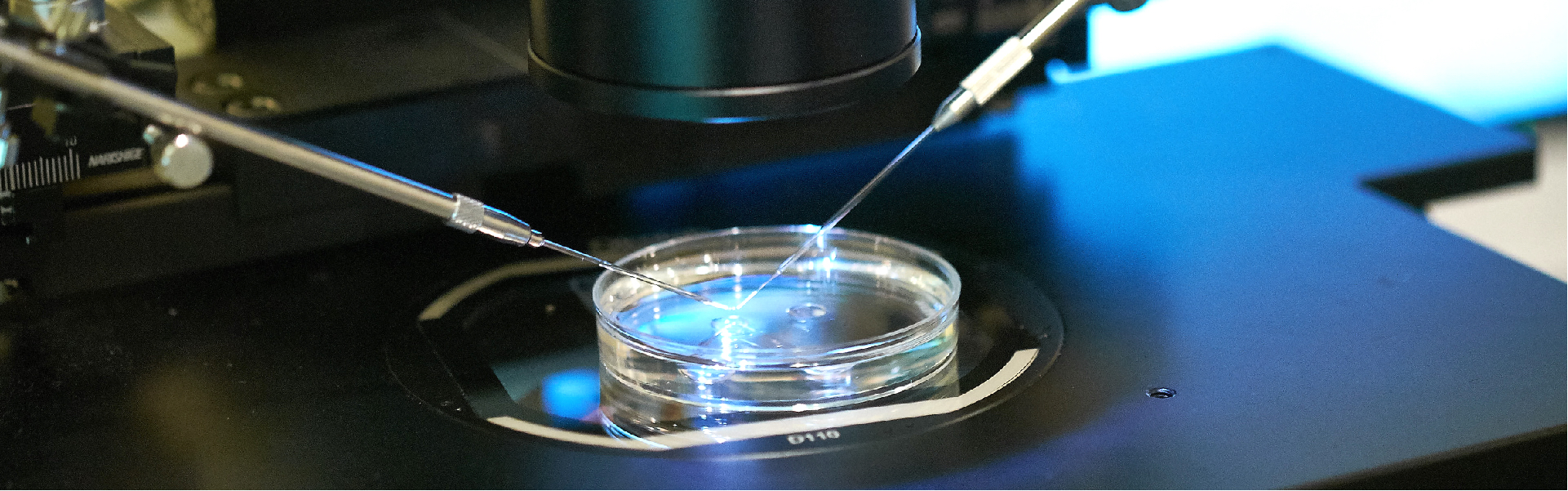
- Using ultrasound for guidance, a thin needle is passed through the top of the vagina and into the ovarian follicles. The needle enters the follicles and aspirates or removes the follicular fluid, which contains the eggs. As soon as the eggs are retrieved, they can be identified by an embryologist and placed in a petri dish with a culture medium. The culture medium is designed to mimic your own body’s fallopian tube secretions. This medium nourishes the egg and the subsequent embryo just as your natural bodily secretions would inside your womb.
- The procedure takes approximately 5-20 minutes, depending on the number of follicles you have.
When the procedure is over
- You will wake up easily and comfortably
- Most women do not have any discomfort beyond some mild cramping
- Before you leave, you will know how many eggs were retrieved and the quality of the semen sample before you leave.
- After you feel comfortable walking (usually 30-45 minutes), our nursing staff will review discharge instructions with you and your partner. You will be escorted to your vehicle to proceed home.
- Please have extra strength Tylenol at home for discomfort.
- You will likely experience cramping in your lower abdomen and/or up under your ribs. Rest, Tylenol, and hydration are important for self-care at home.
- You will likely be given instructions for daily progesterone to supplement your own. This additional progesterone starts the day after egg retrieval and continues for at least two weeks. Progesterone is a hormone which transforms the lining of the uterus to be an ideal receptor for the embryos.
- The next day a member of our team will call you to review how many eggs we were able to inject with sperm and how many fertilized. If you have not already decided to do a frozen transfer by this time, a final decision will be made regarding a fresh (if possible) vs. frozen transfer.
- If doing a freeze all, you will receive a final update of your embryos on or around day 7 of embryo development.
- If a fresh transfer is chosen: The day after your egg retrieval, we will schedule your embryo transfer. This may be 2-5 days after your egg retrieval.
The Embryology Lab: Step 3 of the IVF Process
While the patients themself are not involved in the lab part of the In Vitro Fertilization process, their eggs, embryos, and sperm are. And if doing a fresh embryo transfer, they will be preparing their body for transfer while their embabies are in the lab. If doing a freeze all cycle with a frozen embryo transfer, the intended parents will likely be resting and recovering while the embryologists take good care of the developing embryos.
That said, the ongoing of the embryology lab can be broken down into two main parts:
- Fertilization
- Embryo Development
Fertilization
Generally speaking, there are two types of fertilization used in In Vitro Fertilization:
- Conventional IVF Fertilization: In conventional fertilization, the embryologist adds sperm directly to the culture dish containing the eggs. The sperm then attach to the outer portion of the egg (the zona) and attempt to penetrate the shell. Because the sperm and egg are in relatively close proximity, this can work for many people, including patients with mild male factor infertility.
- Intracytoplasmic Sperm Injection (ICSI): With ICSI fertilization, a single motile sperm is singled out using a microscope in the embryology lab. Its tail is then carefully scrambled by the embryologist in order to safely allow its injection directly into the egg. The embryologist then sucks that prepared sperm into a very small hollow needle, which is then plunged into the egg and injected into the egg. This is generally highly recommended (or required) for those with severe male factor infertility, but it is widely practiced in many clinics (including CNY) regardless of any male factor infertility as a way of ensuring fertilization.
Embryo Development
After fertilization, the embryos (fertilized eggs) are placed inside an incubator, which serves as a sort of “artificial fallopian tube” (early development normally takes place in the fallopian tube) during early embryonic development. Maintaining a proper environment that mimics the Fallopian tube/uterus is absolutely critical to embryo development.
Embryos develop inside the embryo incubators for up to 7 days – until they reach a cleavage or blastocyst stage of embryonic development.
The Embryo Transfer: Step 4 of the IVF Process
The embryo transfer is a simple procedure that takes only a few minutes and is relatively pain-free, like an intrauterine insemination, pap smear, or speculum exam at the ob-gyn. No anesthesia or recovery time is needed.
There are many different types of embryo transfers – but from a patient’s perspective, there are really only two types that have a significantly different process: a fresh embryo transfer and a frozen embryo transfer.
The Process of Preparing for a Fresh IVF Embryo Transfer
Fresh embryos can be transferred 2 through day 7 after the egg retrieval, but are usually transferred as a cleavage stage embryo on day 3 or as a blastocyst (blast) stage embryo on day 5. As you can see in the example below, the embryo transfer takes place on day 17, 5 days after the egg retrieval and thus would most likely be a blastocyst stage transfer.
The Days Leading Up to the In Vitro Fertilization Transfer
As you can see in the calendar above, two medications (estrogen & progesterone) are usually started the day after the egg retrieval and continued every day until the pregnancy test (and further if pregnant). After the egg retrieval, most women are able to resume their daily activities, however, it is important to avoid any strenuous exercise and give your body time to heal, rest, and prepare for implantation.
The Day of the In Vitro Fertilization Transfer
- The morning of the embryo transfer the patient will most likely be instructed to take their usual medications, including vaginal suppositories.
- The patient may also eat, drink, and shower. LEAVE YOUR WATCH OR JEWELRY AT HOME. IT IS IMPORTANT THAT YOU AND YOUR CLOTHING NOT SMELL OF HAIR SPRAY, PERFUME/COLOGNE, OR TOBACCO SMOKE. (This applies to anyone accompanying you into the procedure.)
- Although it is not necessary, we generally recommend that someone drive you to avoid all possible stress. IF YOU ARE TO RECEIVE VALIUM BEFORE THE PROCEDURE PLEASE BRING SOMEONE WITH YOU WHO WILL BE ABLE TO RECEIVE INSTRUCTIONS FOR YOUR CARE FOLLOWING THE PROCEDURE AND PROVIDE YOU WITH TRANSPORTATION AFTER THE PROCEDURE
- Your partner, if applicable, is welcome to be in the room with you during your embryo transfer.
- If desired, you can choose to do acupuncture and or intralipids prior to transfer.
- We recommend having a slightly full bladder for embryo transfer. Do not urinate within 30 minutes of coming to the office.
- On the day of your transfer, one of our practitioners, along with the embryology team, will examine the embryos to determine the best embryo to transfer. By the time of your transfer, we will have reviewed the quantity and quality of embryos made as well as the number of embryos that you would like to have transferred.
The IVF Embryo Transfer Process
Upon arrival to your embryo transfer room, you will meet with a member of our nursing team who will be with you for your transfer. You will also meet with the physician. During the transfer, the embryos are “loaded,” into the tip of a catheter along with a very small amount of transfer medium. The physician, along with a member of the embryology team and a nurse will confirm the patient’s identity to ensure the embryos are properly matched.
The catheter is then gently passed through the cervical canal and into the uterus using an abdominal ultrasound to provide visual guidance during the transfer. The embryos are slowly expelled near the top of the uterus. After carefully removing the catheter, an embryologist will double-check that the embryos indeed left the catheter using a microscope.
The embryo transfer does not require anesthesia but we will provide a Valium 5mg by mouth on arrival if desired.
After the Embryo Transfer
You will rest on the transfer bed for approximately 15 minutes.
During this time we will review post-transfer instructions including scheduling the pregnancy tests or instructing when to make those appointments with a local provider if coming from out of the area. This date will be calculated depending on the “age,” of the embryo, but is generally two weeks after the egg retrieval.
After this rest period, you will have your acupuncture treatment or be discharged to home.
We do recommend that you rest for the remainder of that day, getting up to use the bathroom and for meals only.
The Process of Preparing for a Frozen IVF Embryo Transfer
Unlike a fresh transfer, the process of a frozen transfer cycle is solely dedicated to preparing the body for transfer. That is, no stimulation medications, no egg retrieval.

The process for a FET cycle starts the same way as any fertility treatment cycle: call the clinic on day one of your menstrual cycle. If you don’t have any or they are infrequent, you will likely be instructed to call the office whenever you are ready. Once that happens, the process is quite different (at least until around day 13 of medications – the day after retrieval of a fresh transfer cycle)
The Process of Preparing the Uterine Lining for Transfer
You will come into the office on day 2-4 of your menstrual cycle for the baseline appointment and cycle instructions (this is “Day 1” of the treatment in the calendar above). That same day you will begin estrogen medications and be told to schedule a monitoring appointment for around 7-10 days later. If all goes accordingly (the uterine lining is developing just as it should) you will be instructed to add progesterone to your daily medication list starting a day or two after that monitoring appointment. Of course, it is very possible that you need to come in for another monitoring appointment to check the lining again before receiving instructions as to when you will start progesterone.
If the frozen embryo is a blastocyst, the transfer will be scheduled on the 6th day of progesterone. If the frozen embryo is at its cleavage stage, the embryo transfer will be scheduled for the 4th day of progesterone.
The FET IVF Embryo Transfer Process
The process the day of a frozen embryo transfer is the same as a fresh embryo transfer. Please see the above.
The “Two Week Wait” and Post Transfer Care
While the IVF treatment technically ends with the embryo transfer, you will likely continue medications to help support implantation and pregnancy.
Below is a general schedule of what that might look like:
- Day 17: Embryo Transfer + progesterone + estrogen
- Day 18: progesterone + estrogen
- Day 19: progesterone + estrogen
- Day 20: progesterone + estrogen
- Day 21: progesterone + estrogen
- Day 22: progesterone + estrogen
- Day 23: progesterone + estrogen
- Day 24: Blood Test + progesterone + estrogen. This blood test will be performed to determine if your hormone levels are within the expected range. This can be done at any lab of your choice if not local to CNY offices. Your results should be available the same day.
- Day 25: progesterone + estrogen
- Day 26: Pregnancy Test + progesterone + estrogen. About two weeks after the egg retrieval, a blood test will be performed to determine if you are pregnant. This can be done at any lab of your choice. Your results should be available the same day.
Things to keep in mind during the two-week wait:
- Drink plenty of non-caffeinated beverages. Avoid sugar and artificial sweeteners. Eat plenty of fat
- Continue acupuncture or massage
- Reduce stress. Do things that make you happy. Maintain a positive outlook!
- Abstain from any high impact/intensity exercise. Stick to walking and yoga.
- No heating pads or hot tubs
- You may resume sexual activity
- Continue all of your medications as directed including your prenatal vitamin.
- Do not start any new medications or take anything over the counter without consulting our office.
Things you may or may not feel during the two-week wait
- You may be constipated; this is normal. You should increase your fluids and fiber intake. You may take a stool softener or fiber supplement.
- You may be tired or fatigued. This is normal; your body is preparing for pregnancy. Get plenty of rest!
- You may have some spotting. You do not need to be concerned. Call the office if the bleeding is heavy like a period.
- You may still feel bloated and have some mild cramping. Take Extra Strength Tylenol as you need it. Follow the instructions on the bottle. If the pain becomes severe call the office.
If the pregnancy test is positive
If the pregnancy test is positive, we will repeat the pregnancy test in 2-3 days to evaluate your rising levels. An ultrasound will be scheduled approximately one week later to determine the implantation site and a growing gestational sac. The heartbeat should be seen by 6 weeks gestation.
Once a heartbeat is detected, there is a 90-95% probability that the pregnancy will continue to a live birth. IVF pregnancies are no higher a risk than natural pregnancies. At about 12 weeks into your pregnancy, you can return to your obstetrician for routine prenatal care.
If the pregnancy test comes back negative
If the pregnancy test is negative
we will instruct you on what medications to stop and what medications you may continue. Your period should start in a few days. You can begin another IVF cycle as soon as you like.
Your Cycle Report
Within two weeks of your retrieval, in your patient portal, there will be a summary from our embryology team with the details of your most recent IVF cycle. It will outline the number of eggs retrieved and their disposition. Not all embryos will continue on to be transferred or cryopreserved (frozen). There will be a column indicating how many embryos were transferred, how many embryos were cryopreserved, and how many embryos were discarded. Embryos are discarded when their development has arrested.
The IVF Process Summary
If you made it this far, congratulations! You’re either an expert and know everything about the IVF process, or you’re a little bit overwhelmed by too much knowledge. So let’s wrap things up with a nice little recap of what the IVF process looks like one more time. IVF, is an incredibly complex medical treatment that has many ifs and variables and many, many steps. But, if you want to put your mind at ease tonight and rest easy just think of the IVF process as a main four steps encountered in this article:
- Ovarian Stimulation
- The Egg Retrieval
- The Lab
- The Embryo Transfer
Most importantly, it’s important to remember that each and every person is unique and will have differences (either small or fairly substantial) throughout the IVF process. The good thing is that you’ll have a fertility doctor, a team of amazing nurses, and a host of other supporting staff guiding you every step of the way,
And, if you’re new here and still looking for experts to lead you on your path to parenthood, we are here and happy to help. If you’re ready, feel free to schedule a consultation