Male Factor Infertility
Male infertility affects at least 30 million men worldwide. Infertility in men is defined as the inability of a male to make a fertile female pregnant after a minimum of one year of unprotected intercourse.
According to multiple sources, males are solely responsible for 20-30% of infertility cases and contribute to 50% of cases overall. Interestingly, Dr. Magarelli states the current medical consensus is that approximately 60-70% of all cases that enter a fertility clinic are due to male factors. This is due to the fact that infertility is treated heavily at OBGYNs (a doctor for females) before being referred to a fertility clinic. Men on the other hand, are rarely treated prior to entering a fertility clinic.
Because males contribute to such a large portion of infertility cases, we highly recommend that both male and female partners (if applicable) undergo fertility testing before beginning fertility treatment.
Male fertility can easily be evaluated via a semen analysis and further examined if necessary. Male Fertility testing can save you thousands of dollars in treatment costs and help guide you and your fertility specialist in determining proper fertility treatment.
This article will discuss all aspects of male infertility, including common causes, male fertility testing, fertility treatments, and ways to boost male fertility.
Fast Facts
- 4-12% of men experience infertility.
- 30 million men worldwide experience infertility.
- Male fertility can be affected by many lifestyle factors like smoking, alcohol consumption, illicit drug use (like marijuana), diet, and more.
- Fertility medications like Clomid have been shown to improve certain aspects of male fertility.
- Male fertility supplements, eating a fertility diet, and making lifestyle changes like exercise may help to boost male fertility.
What is Male Infertility?
Male infertility is defined as the inability of a male to make a fertile female pregnant after a minimum of one year of unprotected intercourse.
How Common is Male Infertility?
4-12% of all men experience infertility; that’s roughly 30 million men worldwide.
When a couple experiences infertility, male infertility is equally as likely to be the cause as female infertility.
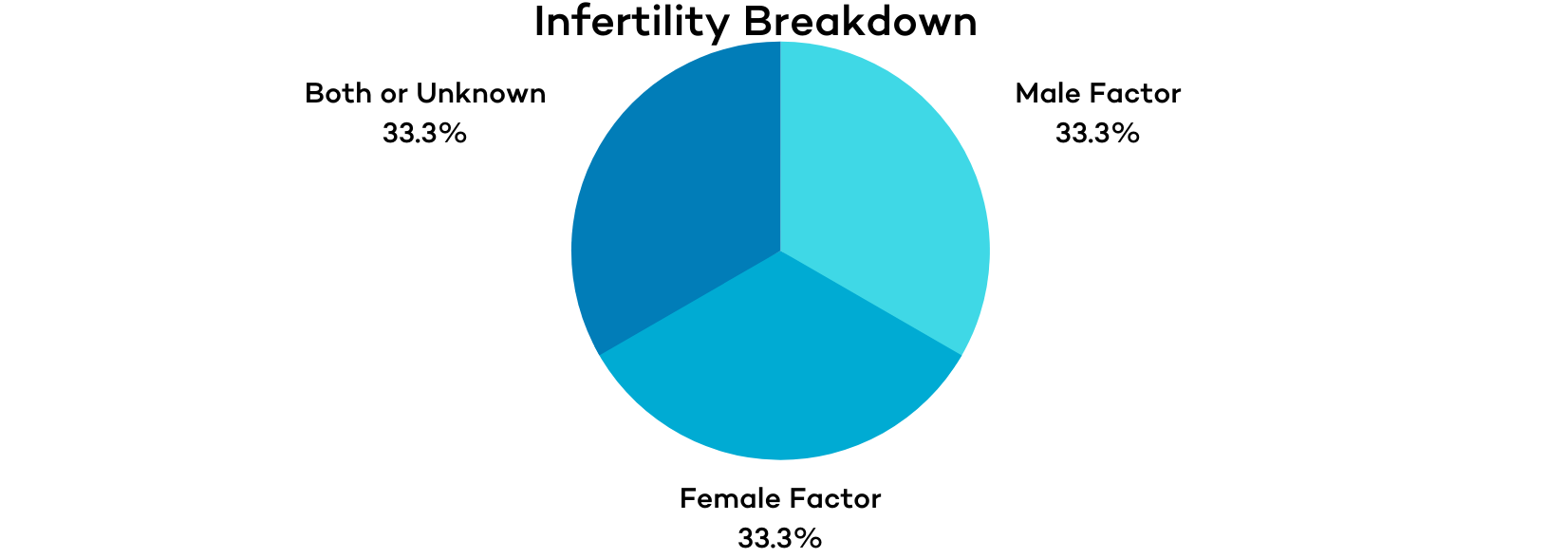
Approximately 1/3 of infertility cases can be attributed to male infertility, 1/3 to female infertility, and 1/3 to unknown causes or a combination of male and female infertility.
That said, once a couple reaches a fertility clinic, it is far more common that male factors are an issue. According to Dr. Magarelli, the current medical consensus is that approximately 60-70% of cases treated inside a fertility clinic are due in part or in full to male factors.
This is due to the fact that female infertility is heavily treated (and often successfully) at the OBGYN level before being referred to a fertility clinic. Men, on the other hand, are rarely treated prior to entering a fertility clinic.
This results in a great deal of easily managed female infertility cases being “cured” and relatively few male cases being “cured” before entering a fertility clinic.
Male Infertility Symptoms
Most men with infertility don’t experience any “symptoms” in the way we typically think of them. The most typical “symptom” of infertility in men is the inability to conceive. Inability to conceive is oftentimes tied to other male infertility “symptoms” like inadequate spermatogenesis (sperm production), low sperm count (number of sperm), irregular morphology (sperm shape), and impaired motility (sperm movement).
Some men’s infertility may be caused by or contributed to by an underlying health condition like an inherited disorder, dilated veins near the testicle, or blockages that prevent the passage of sperm may cause observable symptoms like the following:
- Erectile dysfunction or impaired sexual performance
- Pain or swelling in the testicles or testicular area
- Gynecomastia (abnormal breast growth)
The symptoms listed above and others associated with infertility are commonly associated with low testosterone levels or other hormonal imbalances.
What is Required for a Man to Be Fertile?
1.) Production of healthy sperm. – At least one testicle must function properly, and the body must produce hormones like estrogen and testosterone, which are required for sperm production.
2.) Sperm must be present in the semen. – The testicular tubes must function properly so that sperm can be carried from the testicles to mix with semen and be ejaculated.
3.) An adequate amount of sperm in the semen. – The lower the sperm count, the lower the chances for conception. A minimum amount of sperm must be present in the semen to reach and fertilize the partner’s egg.
4.) Sperm must be functional and able to move. – If sperm have poor motility or morphology, they will not be able to swim correctly and reach the egg.
What Causes Male Infertility?
As mentioned above, male infertility isn’t usually caused by, but it is commonly tied to the following four main “symptoms” or issues:
- Inadequate spermatogenesis (sperm production)
- Low sperm count (number of sperm)
- Irregular morphology (sperm shape)
- Impaired motility (sperm movement)
These issues can have many different causes and contributing factors. Male fertility issues can be caused or contributed to by all of the following:
Health and Lifestyle Causes –
Medical Causes –
- Cancer
- Medication side effects
- Hormonal disorders
- Androgen insensitivity
- Androgen excess State
- Estrogen excess state
- Testicular Failure
- Congenital or developmental testicular disorder (e.g., Klinefelter syndrome)
- Testicular Trauma
- Varicocele
- Obstruction of the reproductive tract
Environmental Causes/Other –
Common Male Infertility Diagnoses
Azoospermia
Azoospermia is the medical term used to describe when there is no sperm present in a man’s ejaculate. The absence of sperm in the ejaculate affects 15% of infertile men.
An azoospermia diagnosis has two classifications (1) obstructive azoospermia (OA) or (2) non-obstructive azoospermia (NOA).
Obstructive azoospermia –
OA is defined as the absence of sperm in the ejaculate despite normal spermatogenesis (sperm production). It results from obstruction at any location between the testis and the ejaculatory ducts.
OA can be caused by infection, congenital anomalies (body structure or function abnormalities), inflammation, or past medical treatments/surgeries (like a vasectomy). It is diagnosed through a combination of history/physical examination, laboratory testing, genetics, and imaging studies.
Oftentimes, OA can be treated through corrective surgery or vasectomy reversal. Couples where the man has OA can get pregnant without corrective surgery by utilizing a sperm retrieval procedure and in-vitro fertilization (IVF) or intracytoplasmic sperm injection (ICSI) IVF. (More information on IVF and ICSI IVF is below.)
Non-obstructive azoospermia –
NOA is defined as no sperm in the ejaculate due to failure of spermatogenesis. It is considered the most “extreme” cause of male infertility. NOA has been estimated to affect 1 in 100 men.
NOA is caused by a hormone abnormality that doesn’t stimulate the testis to produce sperm, or because of an intrinsic defect in the testicles. It is identified through clinical assessment (testis consistency/volume), laboratory testing (FSH), and genetic testing (karyotype, Y chromosome microdeletion, or specific genetic testing for hypogonadotropic hypogonadism).
Patients with NOA can also conceive using their own gametes by undergoing a sperm retrieval procedure and ICSI IVF. Research indicates that testicular sperm retrieval is successful in up to 50% of men with NOA.
Oligospermia
Oligospermia is defined as a low or reduced count of sperm in the semen (low sperm concentration). men with oligospermia have less than 20 million sperm per milliliter of semen. Low sperm concentration affects 25% of infertile men.
Men with oligospermia often experience poor sperm motility and morphology, indicating poor spermatogenesis. The vast majority of oligospermia cases are unexplained. Still, it can be caused by endocrine dysfunction, anatomic abnormalities, medications, inflammation, or environmental exposures (toxins, heat, etc.).
Oligospermia is identifiable through a basic semen analysis, but a full work-up is required to identify the underlying cause. First, fertility specialists will administer a physical examination, hormonal evaluation, and imaging to eliminate possible reversible factors such as hormonal deficiencies, medication effects, and retrograde ejaculation. Then, after ruling out reversible causes, they will attempt to identify any underlying genetic syndrome through genetic testing or medical reasons through additional evaluation.
Even after a comprehensive work-up, 60% to 75% of cases remain unexplained.
Depending on testing results, different treatments may be indicated. Possible oligospermia treatments include:
- Medication withdrawal
- Gonadotropic therapy
- Clomiphene citrate (Clomid) treatment
- Vitamins and supplements
For men with untreatable oligospermia, fertility treatments like intrauterine insemination (IUI), IVF, and ICSI IVF can be used to achieve conception.
It has been reported that men with oligospermia can achieve 50-75% fertilization rates and clinical pregnancy rates of 20% per cycle when utilizing IVF with ICSI treatment. Research indicates that after three cycles, men with oligospermia have achieved an overall cumulative live birth rate of 50%.
Asthenospermia
Asthenospermia is defined as reduced sperm motility. Men with asthenospermia have less than 40% sperm motility or less than 32% progressive motility. Severe asthenospermia is called teratozoospermia, which is characterized by at least 85% of sperm having abnormal morphology.
Asthenospermia and teratozoospermia affect approximately 20% of men with infertility.
Astheospermia is tested for by utilizing a basic semen analysis. Asthenospermia is caused and contributed to by many different factors, including lifestyle choices, environmental factors (like toxins), sperm structural abnormalities, energy deficiencies, inflammation, oxidative stress, and other factors.
Specific supplements like carnitine, ashwagandha, vitamin C, CoQ10, and omega 3 fatty acids have been shown to support healthy sperm motility and may be used to increase sperm motility.
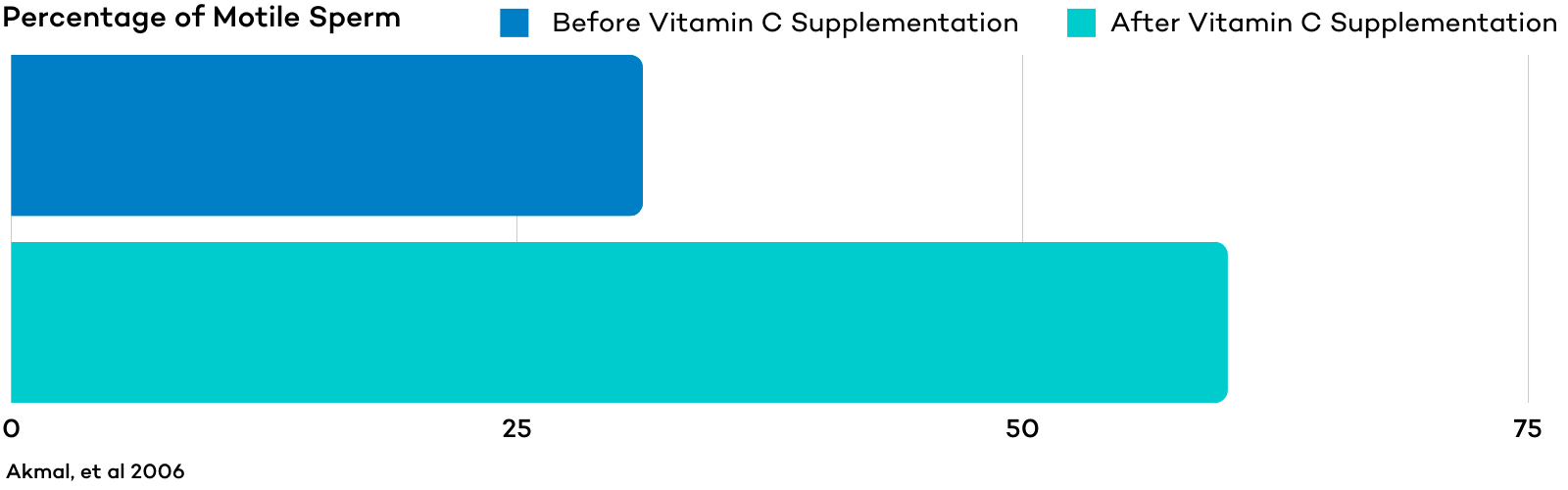
In one study, mean sperm motility increased by 92% from baseline after men received 2 months of vitamin C treatment.
Other natural treatments have also shown promise for improving sperm motility, like acupuncture. Research has indicated that acupuncture can effectively improve sperm motility.
Improving sleep, reducing alcohol consumption, stopping smoking, and avoiding intense exercise have also been shown to improve sperm motility.
If asthenospermia or teratozoospermia are caused by structural abnormalities that can not be improved through natural remedies, fertility treatments like ICSI IVF may help achieve conception.
Varicocele
Varicocele is an enlargement of the veins within the scrotum that holds the testicles. Varicocele is present in 40% of infertile men and 15-20% of all men.
Varicoceles can cause abnormal semen analysis, low sperm count, decreased sperm motility, and abnormal sperm morphology. Men with varicocele commonly experience oxidative stress and inflammation, both of which have been associated with infertility.
The precise cause of varicocele is unknown, but it is considered the most common correctable cause of male infertility. Varicocele can not be treated through medicine or other natural remedies. If the varicocele is impairing fertility or causing pain, it can be treated through outpatient surgery. Following surgery, approximately 70% of men experience improved semen parameters, and 40% to 60% have improved conception rates.
IVF with ICSI can help men with varicocele and sperm conditions like azoospermia conceive.
Primary Testicular Failure (Hypogonadism)
Primary testicular failure (PTF), also known as hypogonadism, occurs when the testes fail to produce sperm despite adequate hormonal support. It is a major cause of non-obstructive azoospermia and oligospermia.
Approximately 12% of male infertility cases are caused by primary testicular failure. Primary testicular failure can be caused by testicular injury, radiation, varicocele, gene mutations, and other congenital or acquired disorders. Kleinfelter syndrome (when a male is born with an extra copy of the x chromosome) is the most common cause of primary testicular failure.
Primary testicular failure is usually tested for after other more common causes of infertility have been ruled out. If semen analysis results come back and indicate low sperm count or no sperm in the semen, a fertility specialist will usually ask about medical history, lifestyle, environmental exposures and then administer a physical examination, hormonal testing. If a cause is not identified, then a testis biopsy is utilized to confirm a PTF diagnosis.
Recommended treatment for PFT depends on the underlying cause. If PFT is caused by varicocele, then surgery may be recommended. Otherwise, men with azoospermia and oligospermia may be able to conceive through a sperm retrieval procedure and ICSI IVF.
Male Fertility Testing
There are many types of male fertility testing available. In almost all cases, male fertility testing starts with a semen analysis.
The Semen Analysis
A semen analysis analyzes the health and viability of a man’s sperm. Semen analyses should be performed during a man or couple’s initial fertility consultation or evaluation.
Semen analysis results act as a guide for determining the most effective fertility treatment. By completing a semen analysis, men and couples can save time and thousands of dollars. For example, if semen analysis results indicate low motility or poor morphology, the fertility specialist may recommend Intracytoplasmic Sperm Injection (ICSI) IVF as the first course of treatment instead of starting with Intrauterine Insemination (IUI) or conventional In Vitro Fertilization treatment.
Semen analyses measure all of the following (and sometimes more) to determine sperm viability :
| Concentration: | >20 million sperm per milliliter |
|---|---|
| Volume: | 2-5 mL |
| Motility: | >50% |
| pH: | 7.2-7.8 |
| White Blood Cells: | <5 per high-powered field |
| Progression: | 2+-3+ |
| Red Blood Cells: | 0 per high-powered field |
| Agglutination: | None |
| Morphology: | > 14% normal forms |
It is important to remember that the results of a semen analysis are just a measure of your sperm parameters at one specific time. There are a lot of ways for you to increase your sperm count, motility, morphology, and overall male fertility.
What if Semen Analysis Test Results Are Abnormal?
If semen analysis results come back as abnormal, or if sperm production appears to be an issue, your fertility specialist will likely recommend additional testing.
Additional testing may include:
- Male fertility hormone testing
- Genetic screening for male fertility – most commonly screening for Cystic Fibrosis Transmembrane Conductance Regulator (CFTR) Gene Mutations, karyotype, Y-Chromosome Microdeletions (YCMD)
- Anti-sperm antibody testing (if sperm motility issues)
- DNA fragmentation testing
- Tests for penetration issues like the Acrosome Reaction Test, Sperm Penetration Assay, and Hemizona Assay Test
- Ultrasound imaging
- Varicocele testing
- Testis biopsy
Check out our male fertility testing guide for a full breakdown of available male fertility tests.
Male Infertility Treatments
Intrauterine Insemination (IUI)
Interutinary Insemination (IUI) treatment is commonly used as a first-line treatment for cases of mild or moderate male infertility and men with ejaculate disorders. During an IUI procedure, sperm is collected, concentrated, and deposited into a woman’s uterus.
IUI procedures may help to overcome unexplained infertility and male factor infertility, especially for men with low sperm motility and low sperm volume.
In Vitro Fertilization (IVF)
Research indicates that oligospermia, asthenospermia, teratozoospermia, autoimmunity, and other forms of male infertility can be successfully treated by Invitro Fertilization (IVF). IVF treatment offers the highest success rates and quickest time to pregnancy of any Assisted Reproductive Technology (ART).
IVF can help increase the chances of pregnancy for nearly all infertile men, but it is especially helpful for men with low sperm count, low sperm concentration, and low sperm motility.
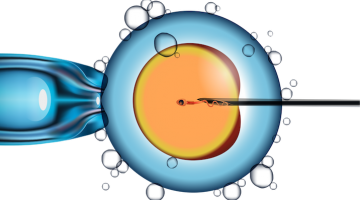
Intracytoplasmic Sperm Injection (ISCI)
Intracytoplasmic Sperm Injection (ICSI) is an advanced reproductive procedure done in an embryology lab during an IVF treatment. A single sperm is injected directly into a woman’s egg to create a fertilized embryo. ICSI procedures can be used as long as viable sperm are present in the ejaculate or retrievable from the reproductive tract.
Research indicates that ICSI treatment can help to overcome severe male factor infertility and allow pregnancy rates up to 52%, with ongoing pregnancy and live delivery rates as high as 37% per IVF cycle attempt.
Sperm Retrieval Procedures
Sperm retrieval procedures are surgical procedures to retrieve sperm from some part of the male reproductive tract. Sperm retrieval procedures like PESA, TESA, and TESE are used when there is no sperm present in the ejaculate. If successful, the sperm retrieved is used with an ICSI IVF procedure.
Sperm extraction procedures can be used after a vasectomy, if a man lacks a vas deferens, or if there is a reproductive tract blockage or insufficient sperm production.
In one study, TESA allowed for high sperm retrieval rates for men with severe oligozoospermia (low sperm count). In the study, sperm was recovered in 90% of men. The recovered sperm was then used in ICSI procedures and produced results that researchers deemed “acceptable.” In this study, the overall clinical pregnancy rate per embryo transfer was 46%.
Testicular Platelet Rich Plasma (PRP)
Testicular Platelet-Rich Plasma (PRP) is a concentrated blood product that contains a high percentage of biomolecules with natural healing and regenerative properties. Testicular PRP is an innovative and experimental technique used on men with azoospermia (zero sperm in the ejaculate) with the goal of achieving even a small number of active sperm in the ejaculate, which can then be used for IVF with ICSI. Here at CNY, Dr. Mariabelle Vardiales is currently conducting research to determine the efficacy of the treatment; so far, the results look promising.
Improving Male Fertility
There are many ways to boost male fertility both naturally and with the use of fertility medications.
Fertility Medications
Male fertility may be improved via oral medications like clomiphene citrate or Letrozole. In addition to oral medications, male infertility can also be treated via injectable medications like human chorionic gonadotropin (hCG) or human menopausal gonadotropin (hMG). The following medications are commonly used to improve several aspects of male fertility.
Clomid (Clomiphene citrate)
Clomid for men is not approved by the FDA so it is prescribed off-label (as clomiphene citrate) to treat male infertility. Clomid is especially useful for men with low sperm counts, but it can also help to improve overall male fertility by correcting hormonal imbalances and increasing testosterone production.
The American Society for Reproductive Medicine (ASRM) published a study on Clomiphene Citrate treatment’s ability to treat men with idiopathic oligozoospermia (unexplained decrease in sperm concentration or quality) and infertility. After 6 months of treatment, the clomiphene citrate treatment group experienced a 36.7% pregnancy rate, nearly three times that of the control group (13%).
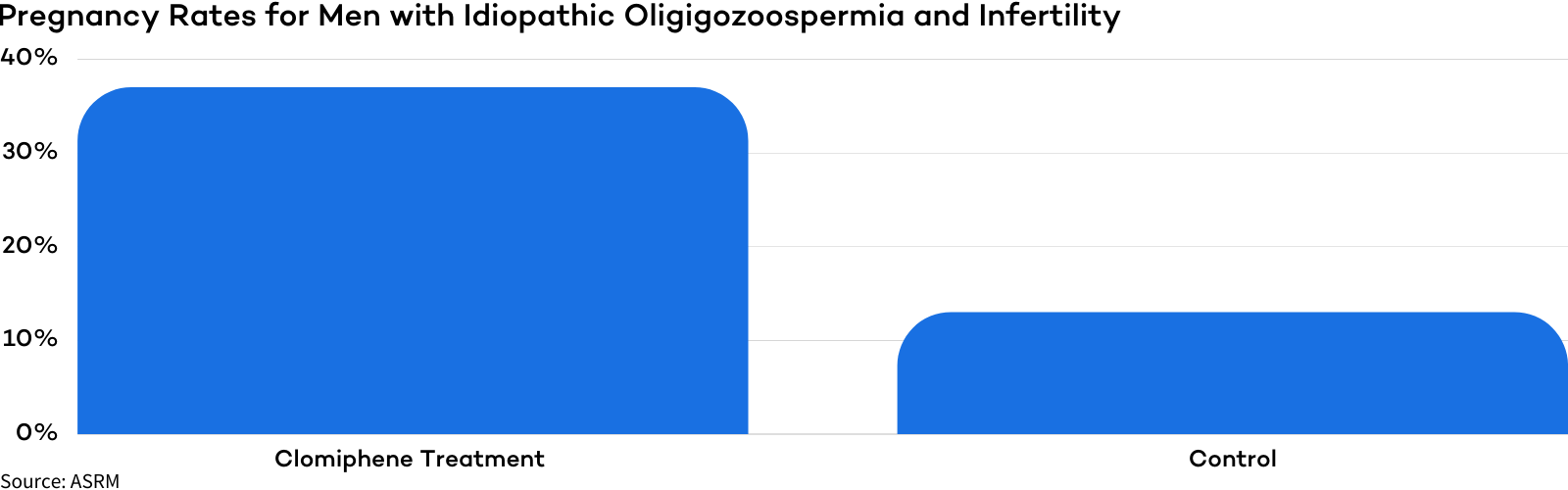
The clomiphene citrate treatment group also saw a greater increase in sperm count and progressive sperm motility when compared with the control group.
Alternative Oral Medications
Letrozole or Femara: Letrozole is a relatively new male fertility treatment that has been demonstrated to improve sperm concentration and the testosterone to estradiol ratio for men with oligozoospermia.
Anastrazole or Arimidex: Recent research has demonstrated that Anastrazole may help to reduce testosterone levels, improve the ratio of testosterone to estradiol, and significantly improve sperm parameters for some men.
Low Dose Naltrexone (LDN)
Lod dose naltrexone (LDN) is used to reduce the symptoms of many medical conditions. LDN is prescribed for male factor infertility due to its anti-inflammatory properties which are believed to encourage better blow flow and nutrient delivery to the developing sperm.
New research has also indicated that LDN may be an effective treatment for men who have erectile dysfunction.
Human Chorionic Gonadotropin (hCG)
hCG has been shown to help induce testis growth, improve spermatogenesis and increase fertility in gonadotrophin-deficient men. Men with low sperm counts and low motility may benefit from daily HCG injections.
Human Menopausal Gonadotropin
If men don’t see results after an extended period of time with hCG treatment, hMG injections may be added to their treatment protocol. In combination, hCG and hMG have been shown to increase sperm count and motility.
Human Growth Hormone (HGH)
Research indicates that HGH may help induce spermatogenesis in men with hypogonadism who are non-respondents to gonadotropin therapy. Growth hormone treatment has also been shown to restore sperm concentration, morphology, and motilit.
Supplements for Supporting Healthy Sperm and Male Fertility
Many different male fertility supplements have been shown to support sperm motility, count, morphology, concentration, overall sperm health, and other aspects of male fertility. Check out some of the best vitamins and nutrients and the aspects of male fertility they support below:
- Vitamin C – sperm count, motility, and morphology
- Vitamin D – hormone production, sperm development, sperm motility
- Vitamin E – sperm motility and morphology
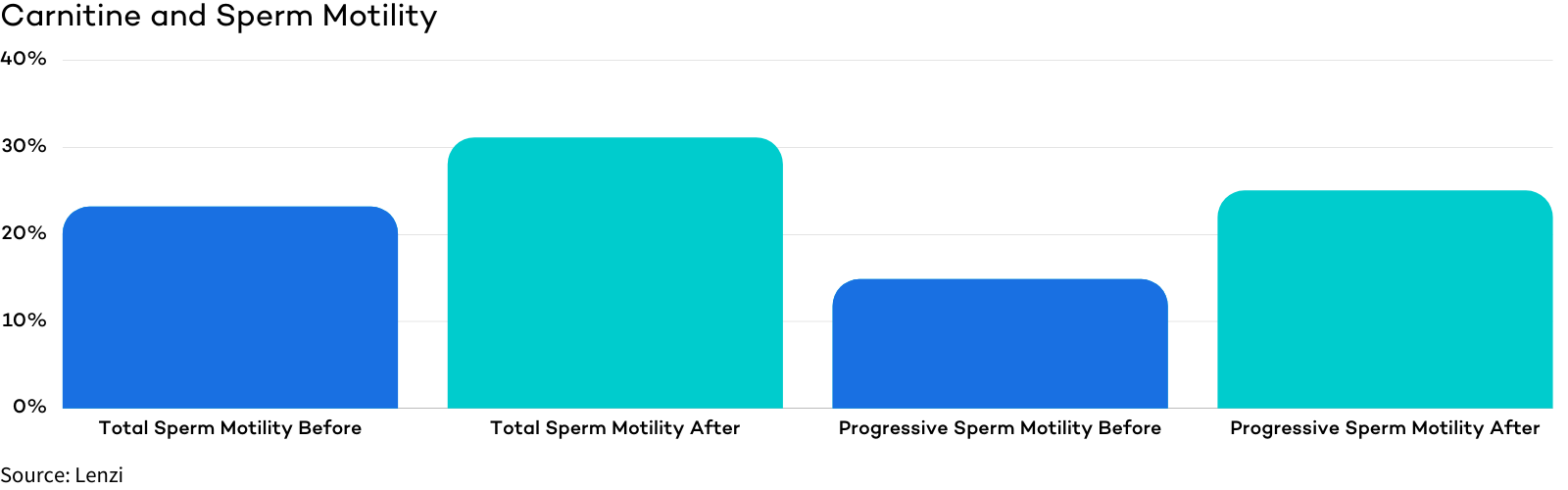
- Carnitine (L-carnitine) – sperm maturation and maturity, all sperm parameters but most significantly sperm motility
- Coenzyme Q10 (CoQ10) – sperm count, motility, morphology
- Folate – sperm count and sperm DNA
- Inositol – sperm motility
- Lycopene – sperm count, motility, or morphology
- Omega 3s – sperm count, motility, and morphology
- Selenium – sperm motility and morphology
- Zinc – sperm development, count, and motility
Supplements Highlights
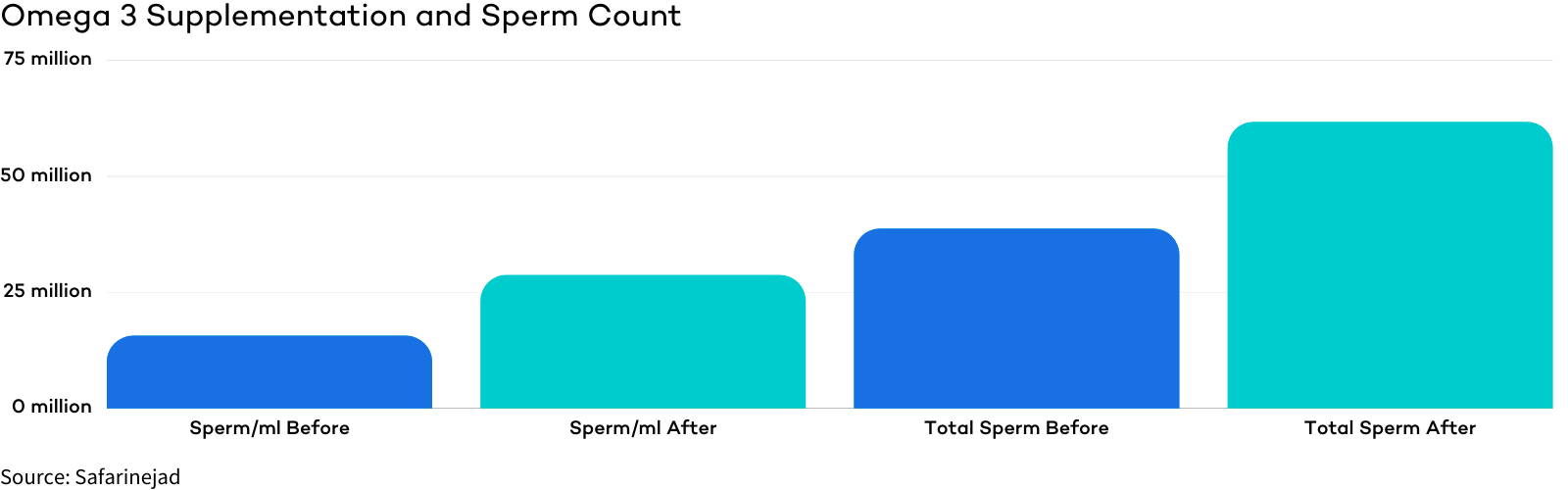
Omega 3s – A study of over 200 men found that after 32 weeks of Omega 3 supplementation those in the treatment group saw an average total sperm count increase from 38.7 million to 61.7 million and a concentration of 15.6 million/ml to 28.7 million/ml.
Carnitine (L-carnitine) – In a study of infertile men who took carnitine supplements for 6 months, the percentage of total motile sperm improved from 23.17% to 31.11% and the percentage of forward progressive sperm went from 14.83% to 25%.
For more information, check out our comprehensive guide on male fertility supplements!
Male Fertility Diet
At CNY Fertility, we believe that the food we eat impacts our fertility, perhaps more than any other single factor. Based on decades of clinical experience, we recommend that men consider eating eat a high fat, moderate protein, and low carbohydrate diet (aka the ketogenic diet). Typical keto foods include fatty meat like ribeyes, pork belly, chicken wings, lamb shoulder, etc. along with butter, heavy cream, coconut oil, and other high-quality fats.
The Ketogenic diet improves male fertility in two main ways, (1) reducing inflammation and (2) improving hormone function.
Acupuncture
Acupuncture is a medical treatment grounded in Traditional Chinese Medicine that involves using sterilized needles to stimulate certain pathways and regulate the flow of energy and blood in the body. Acupuncture is used to treat many different diseases and symptoms. Research has shown that acupuncture causes the brain to release opioids, the body’s natural painkillers, and other endorphins that help moderate stress. Acupuncture is also known to help balance hormone levels.
Specific to male fertility, acupuncture treatment has been shown to be distinctively efficacious in improving sperm quality, especially motility, when combined with traditional Western Medicine. As mentioned above, research indicates that acupuncture may be an effective treatment to improve sperm motility for men with asthenozoospermia.
Stress
Stress and fertility are intimately related. Research indicates that stress may cause or contribute to male infertility, and inversely an infertility diagnosis has been shown to cause and increase stress levels.
Stress can impact hormone production, spermatogenesis, and sperm quality. Men’s stress levels have been demonstrated to significantly increase after diagnosis of male infertility, follow-up appointments, and failed in-vitro fertilization (IVF) treatments.
There are many different proven ways to reduce stress that men can explore.
Yoga is a highly-touted stress-reduction technique that research indicates may cause significant reductions in stress and improvements in several other psychological health measures.
Acupuncture, as mentioned above, has been shown to reduce physiological stress immediately following treatment and over time.
Massage has been shown to reduce stress levels significantly. Massage also offers many additional physical and psychological benefits like improving circulation, reducing muscle tension, encouraging blood flow to the reproductive organs, increasing lymphatic flow, and optimizing reproductive physiology.
Lifestyle Changes
While trying to conceive, you can make many different lifestyle changes to naturally improve your fertility.
Quit Smoking
Smoking negatively impacts nearly every aspect of health and negatively impacts male fertility.
For men, smoking has been associated with reduced sperm density, total sperm count, and the total number of motile sperm.
| Sperm Density | Sperm Count | Sperm Motility |
|---|---|---|
| -15.3% | -17.5% | -16.6% |
Limit Alcohol Consumption
Excessive alcohol consumption impairs men’s sperm quality. Alcohol abuse can result in impaired testosterone production, shrinkage of the testes, sexual dysfunction, and infertility.
Alcohol consumption can also significantly decrease sperm quality, as displayed by the figure below.
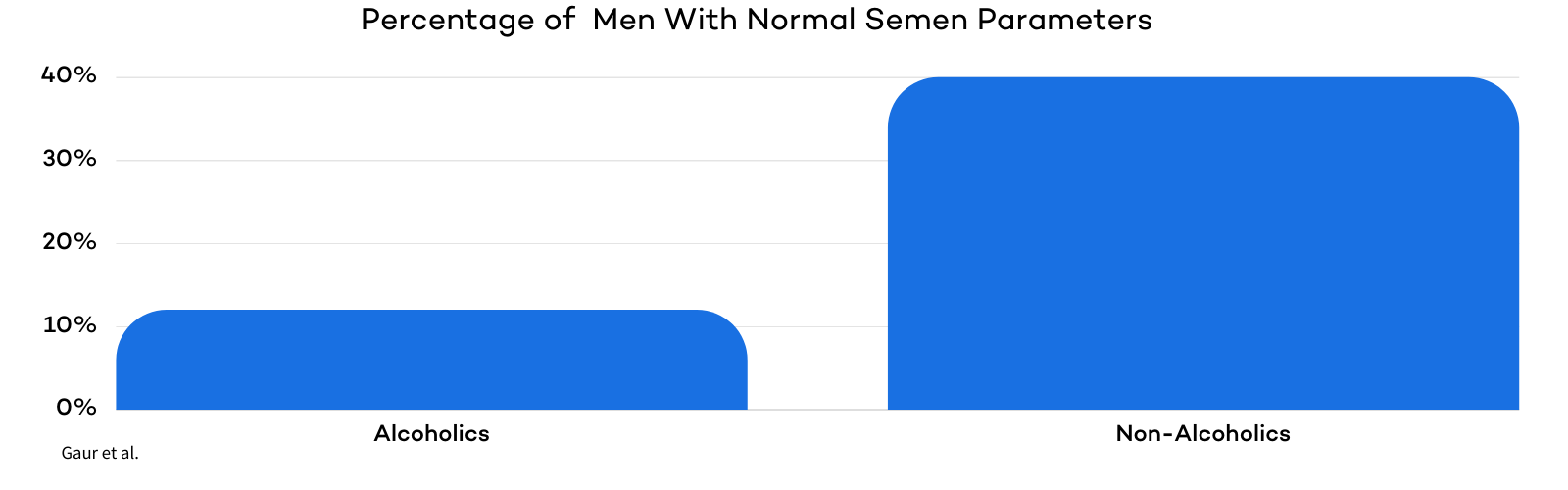
In a study on 100 alcoholics, only 12% had normal semen parameters. Non-alcoholic men were three times as likely (37%) to have normal semen parameters.
Fortunately, stopping drinking alcohol has been demonstrated to quickly and drastically improve semen parameters for heavy drinkers.
Consider Limiting or Stopping Marijuana Use
Several studies exist that link marijuana use to poor sperm quality. In one study conducted in 2015, men who smoked marijuana regularly (more than once per week) had a 28% lower sperm concentration and a 29% lower total sperm count compared to non-marijuana users.
It is worth noting that research is not conclusive, and contradictory studies exist indicating that marijuana does not negatively affect sperm quality. If you have received sub-optimal semen analysis results, you may consider reducing or refraining from using marijuana while trying to conceive. If you use marijuana for therapeutic healing or are prescribed marijuana, you should consult with your doctor to make an informed decision.
Stop Over- Exercising
Moderate exercise is great for fertility. On the other hand, over-exercising can reduce men’s sperm quality and impair fertiltiy.
Research has shown that exhaustive exercise can decrease thyroid hormones, testosterone levels, and overall sperm quality.
Avoid Saunas, Steam Rooms, and Hot Tubs
Heat, mainly from saunas or hot tubs, has been shown to affect sperm production and overall male fertility. Heat stress may cause a decrease in sperm motility and increase the percentage of sperm cells with major and minor defects.
One small study indicates that exposure to hot baths or hot tubs can lead to male infertility.
The Bottom Line about Male Infertility
If you are struggling to conceive or have been diagnosed with male infertility, we hope you know that you are not alone.
Male fertility can be affected in many ways, including by medical, environmental, and lifestyle factors.
Fortunately, as you’ve seen in this article, there are many available treatments to boost male fertility and fertility treatments that can help you conceive.
Be sure to consult with your fertility specialist or if you don’t have one, schedule a virtual consultation with one of our providers to discuss your treatment options.
Now that you’ve read all about male infertility, we highly recommend checking out our comprehensive guide on how to increase sperm count, motility, morphology, and overall male fertility!