Day 3 v.s. Day 5 Embryo Transfer
One of the biggest scientific debates in IVF over the past few decades has been whether to transfer embryos at their cleavage or blastocyst stage. These embryonic stages are typically reached on day 3 and day 5-7 of development respectively. Because of this, they are often referred to as day 3 and day 5 embryo transfers.
As laboratory technologies improve, transferring day 5 embryos has become more and more common. The general stance of the American Society of Reproductive Medicine is that Blastocyst embryo transfers are generally preferential for patients with a good prognosis of success.
However, life is not as simple as always transferring day 5 embryos as a significant percentage of IVF cases do not present with a “good prognosis.”
There are concerns about the risk of developing an embryo for longer in a lab and whether or not it actually gives patients a better shot at achieving a live birth. Because of this, current research does not point to a clear consensus on the definitive efficacy of day 3 or day 5 embryo transfers.
In this article we will explore embryo development, the arguments for both day 3 and day 5 embryo transfers, the success rates of each, as well as how we at CNY Fertility determine when we transfer day 3s and when we transfer day 5s.
Fast Facts
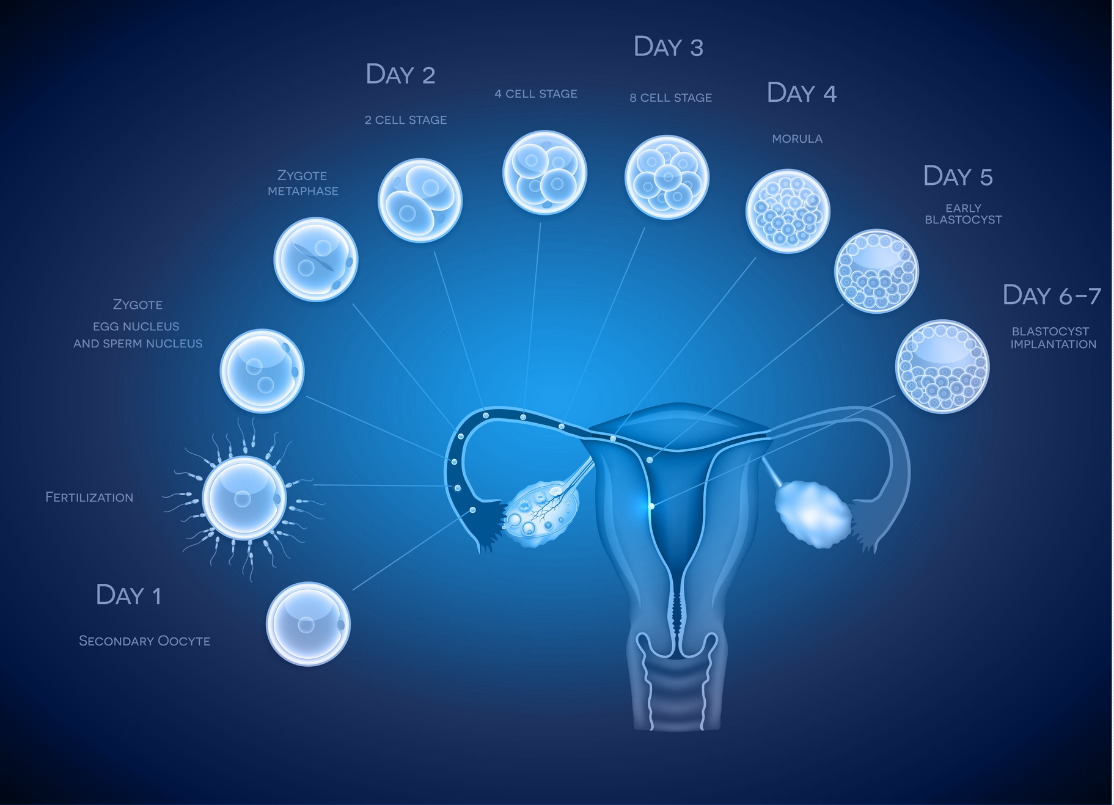
- An embryo begins to develop as a single cell. By day 3, it typically grows into a 6-8 cell “cleavage” stage embryo. Over the next few days, it continues to grow and ideally reaches the blastocyst stage by day 5-7.
- There is significant attrition at every stage of development. For example, a patient may have 10 embryos on the day of fertilization, 5 embryos on day 3, and only 2 embryos on day 5. In fact, some patients may not be capable of making day 5 embryos no matter how many IVF cycles they undergo.
- Because not all embryos continue to develop, patients usually have more embryos available for transfer on day 3 than on day 5.
- Further developed, blastocyst-stage embryos have higher implantation rates, likely due to being more mature and having a higher likelihood of being chromosomally normal.
- While blastocyst embryos have higher implantation rates, cleavage and blastocyst embryos seem to have similar pregnancy and live birth rates on a per IVF retrieval basis. This is because more embryos are available on day 3 so either more embryos can be transferred during a single embryo transfer or there is a higher likelihood of embryos being available for multiple transfers should the first transfer fail.
- Both day 3 and day 5 embryo transfers are based on and supported by sound theoretical and scientific evidence and should both be used depending on the circumstances.
- CNY Fertility supports and practices a well-documented and supported methodology of determining when to transfer day 3 embryos and when to attempt blastocyst culture. If a patient has 5 or more fertilized eggs on day 1, blastocyst culture is attempted; if a patient has 4 or fewer fertilized eggs on day 1, the embryos are usually transferred or frozen on day 3 (unless PGT is being done on the embryos).
Introduction to the Arguments for Both Day 3 and Day 5 Embryo Transfer
There is sound scientific evidence and theoretical framework supporting both day 3 and day 5 embryo transfers. The general argument for each side of the day 3 vs day 5 embryo transfer debate goes like this:
- Pro Day 5: Day 5 embryos are more mature and have therefore demonstrated a higher likelihood of being chromosomally normal and otherwise healthy (if they weren’t they would have died off already). If an embryo has the genetic makeup and “strength” to make it 5 days inside of a lab incubator, it has a better chance of resulting in pregnancy if it is transferred. Because of this, you need to transfer fewer embryos. This keeps success rates high while minimizing the chance of twin or higher-order multiple pregnancies. Similarly, there is better temporal synchronization between embryo and endometrium at the time of a blastocyst embryo transfer since natural implantation after sexual intercourse usually occurs on days 5–7. Day 5 embryos can also be genetically tested, though there is a similarly heated debate as to the efficacy of such a practice and when it should be conducted, if at all.
- Pro Day 3: No matter how good an embryology lab is in mimicking the environment of the uterus, it is still an artificial environment that is not 100% ideal for embryo growth. Embryos that have developed to day 3 have already demonstrated enough genetic normality and resilience to warrant being transferred. Some embryos that could survive in the optimal uterine environment may die off between day 3 and 5 if left in a lab to develop; thus some potentially viable embryos will never even have a shot at life if grown in a lab that long. Despite the negative stigma around day 3 embryo transfers, data shows that transferring day 3 embryos may in fact result in equal or higher live birth rates per IVF retrieval.
Of course, there a many fertility doctors and clinics, like CNY Fertility, who transfer both day 3 and day 5 embryos on a daily basis. So for many, there is no right or wrong side to this debate.
Background info on Day 3 Embryos
By day 3, most embryos have undergone a few rounds of division and are composed of 6 to 10 cells, though they may have as little as 4. Day 3 embryos are referred to as cleavage stage embryos as the embryo cells are dividing but not yet growing in size.
There are some large-scale studies that suggest embryos comprising 8 or more cells by day 3 have significantly higher live birth rates than day three embryos with less cells.
Background info on Day 5 Embryos
By day 5, embryos begin to reach the blastocyst stage of development. Blastocyst embryos divide and increase their number of cells rapidly. Cells also begin to specialize and divide into the inner cell mass (which develops into the fetus) or the trophectoderm epithelium (which develops into the placenta and other tissues the body needs for pregnancy.)
Growing embryos until they reach the blastocyst stage can be a useful selection tool for choosing higher-quality embryos as healthier embryos have a higher chance of become blastocysts.
Success Rate Comparison
As mentioned directly above, growing embryos for 5 days may allow embryologists to identify high-quality embryos for transfer and allow for theoretically better embryo uterine synchronicity, but does it matter?
In a study published in Human Preproduction in 2000, 201 women were randomly assigned into day 3 and day 5 transfer groups. In both groups, 2-3 of the highest-graded embryos belonging to each patient were then transferred.
The implantation rates for each individual embryo were slightly higher for the day 5 transfer group (24%) compared to the day 3 transfer group (21%), but because slightly more embryos were transferred on average for the day 3 group, the pregnancy rates were the same for both groups at 39%.

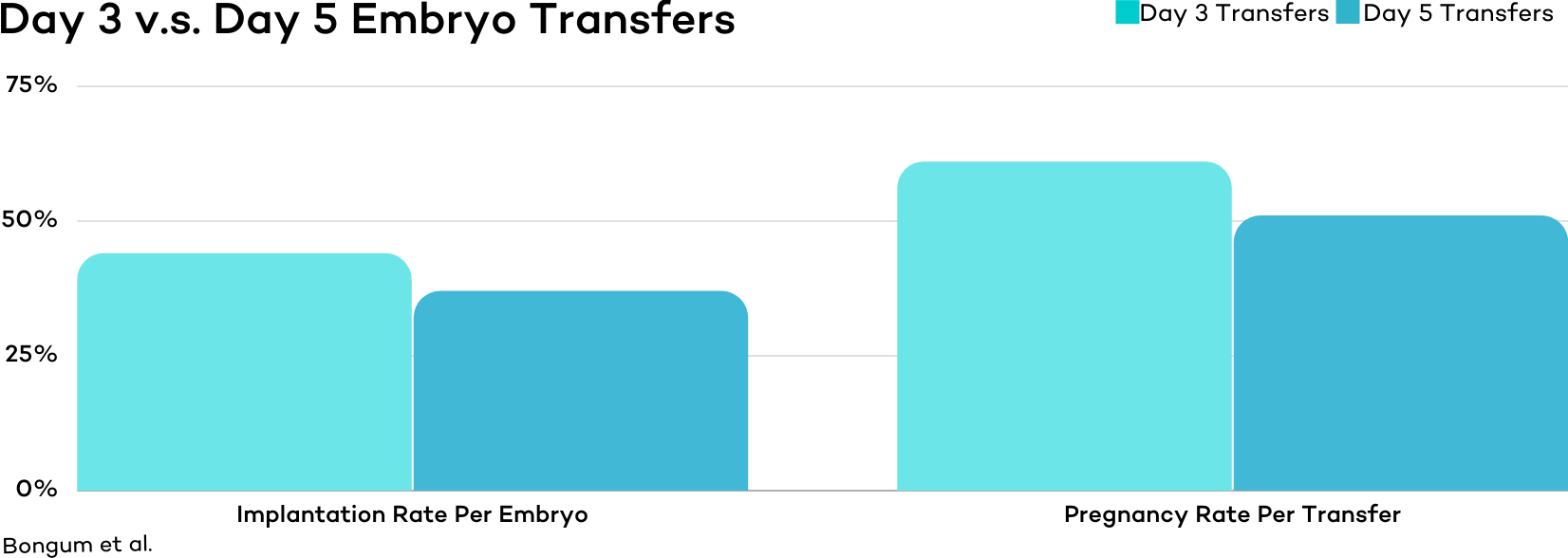
Though results were statistically insignificant, another study out of Denmark published in 2003 actually found that Day 3 Embryos (that had at least 8 cells) have slightly better outcomes compared to blastocyst embryos.
In this study, implantation rates were 44 versus 37% and clinical pregnancy rates were 61 versus 51%, .
Yet another study conducted in 2017 found similar results. In this study, researchers randomly assigned 190 women into either day 3 or day 5 transfer groups in one study and obtained the following results.
| Measure | Day 3 Transfers | Day 5 Transfers |
| Implantation Rate | 47.4% | 45.3% |
| Clinical Pregnancies | 46.3% | 44.2% |
| Live Births | 36.8% | 34.7% |
Interestingly, even one of the most heavily cited articles on the topic which ASRM uses in its case for the preferential transfer of blastocyst embryos does not yield statistically significant differences for pregnancy rate; in the study, pregnancy rates of day 3 vs day 5 transfers were 66% and 71% respectively. However, there were significant differences in implantation rate, 30% vs 50%. That means in order for pregnancy rates to be the same, more embryos were transferred at a time when doing a day 3 transfer. The good news is that on day 3, there are more embryos available so needing to transfer more embryos is not of much concern.
| Day of Transfer | Day 3 Cleavage | Day 5 Blastocyst |
| Number of Embryos Transferred | 2.2 | 3.7 |
| Implantation Rate | 30% | 50% |
| Clinical Pregnancy Rate | 66% | 71% |
That said, there are other studies that support day 5 superiority.
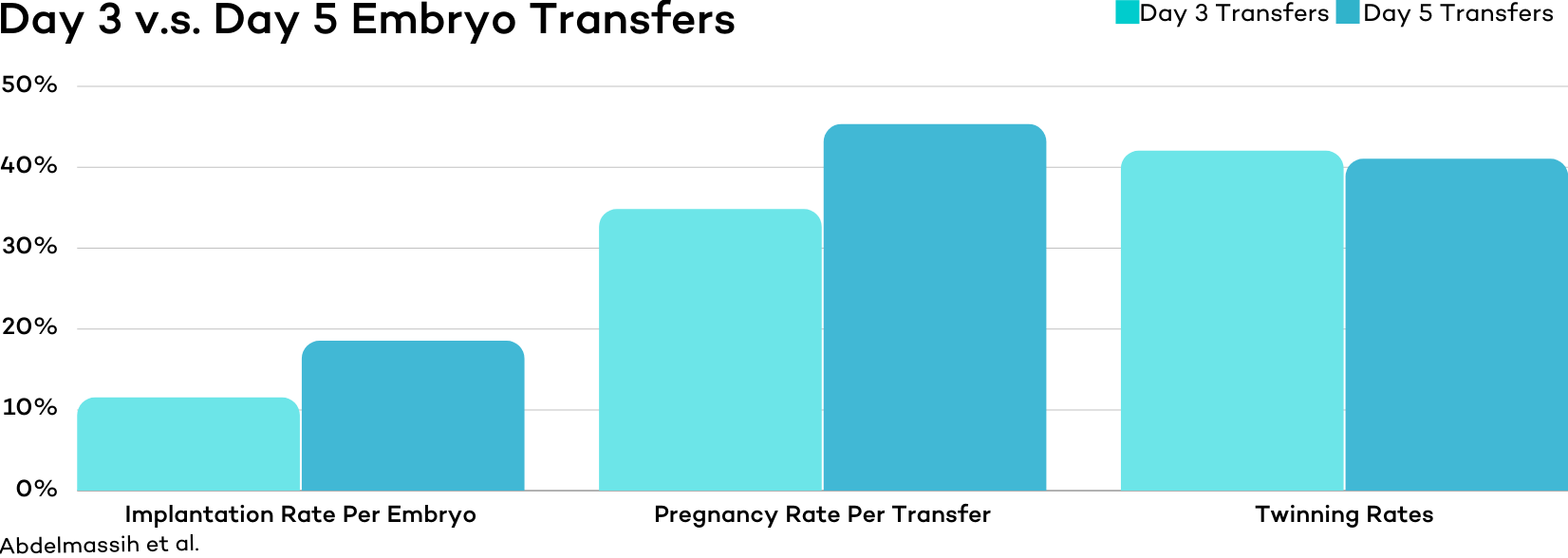
One study conducted at a private fertility clinic found the day 5 transfer group experienced higher implantation and pregnancy rates and lower rates of multiple pregnancies. Pregnancy rates were 34.8% versus 45.3%, implantation rates were 11.5% versus 18.5%, and multiple gestation rates were 47.1% versus 28.5%. .
Another study published in Fertility and Sterility in 2008 found a slight superiority for day 5 embryos when transferring just one of either.
| Measure | Day 3 | Day 5 |
| Clinical Pregnancy | 44% | 52% |
Another heavily cited article published in the New England Journal of Medicine looked at 351 infertile women under 36 years of age. In this study, the researchers noted a significant difference in favor of blastocyst transfers 32.0 percent vs. 21.6.
As you can see, there is quite a bit of evidence supporting both sides.
A large-scale meta-analysis conducted in 2016 looked at 27 controlled studies involving 4031 couples did an excellent job of parsing through the data and providing some much needed clarity.
In this meta-analysis, they found “low quality evidence for live birth and moderate-quality evidence for clinical pregnancy that fresh blastocyst stage transfer is associated with higher rates than fresh cleavage-stage transfer [on a per transfer basis]. There was no evidence of a difference between the groups in cumulative pregnancy rates derived from fresh and frozen-thawed cycles following a single oocyte retrieval, but the evidence for this outcome was very low quality.”
Basically, there it is likely there is some improvement when transferring blastocysts if looked at on a per transfer basis, but if you add up all the transfers from a single retrieval there is likely little to no difference in live birth rates.
The Advantages and Disadvantages of Day 3 Embryo Transfers
Advantages
- more embryos available for transfer, though a higher % are likely genetically abnormal
- embryos placed in the uterine environment earlier
- lower chance of cycle cancelation (due to no embryos being available for transfer)
- similar live birth rates
Disadvantages
- Lower implantation rates per transferred embryo (but there are more embryos to work on day 3 as compared to day 5)
- Because you have to transfer more embryos (which by random chance may both be very healthy embryos) at a time to obtain equal success rates, there is a higher chance of twin or higher multiple pregnancies
- less information available from embryo grading and on embryo quality
- No genetic testing options are available
The Advantages and Disadvantages of Day 5 Embryo Transfers
Advantages
- ruling out embryos that don’t make the blastocyst stage
- higher quality embryos are identified for transfer meaning fewer embryos can be transferred at a time
- higher implantation rates
- May need to go through less embryo transfer to achieve live birth
- Pre-implementation genetic testing is available
Disadvantages
- higher chance that embryos will not survive to transfer day resulting in fewer total embryos available for transfer, or possibly none at all
- higher risk of cycle cancelation
- embryos placed in the uterine environment later
- viable day 3 embryos may not make it to day 5 for transfer
- not a viable solution for patients who don’t produce many embryos
- some people are not capable of producing day 5 embryos
The CNY Way
As you can see by the mixed data displayed in this article, it is very difficult, even for well-controlled randomized studies, to determine if day 3 or day 5 transfers result in superior live birth rates and when to utilize cleavage vs blastocyst embryos.
Even so, the general consensus is that day 5 transfers result in slightly higher live birth rates per embryo transfer.
But not all patients are capable of making blastocyst embryos. That means for some, trying to develop blastocyst embryos would result in a 0% chance of a live birth.
Because of this, there is a need to develop some sort of system for determining when embryos are transferred or frozen on day 3 or allowed to develop longer with the hopes of becoming blastocysts.
CNY Fertility’s policy for determining if a blastocyst culture is attempted is based on the number of thriving day 3 embryos the patient makes. If the patient has 5 or more fertilized eggs on day 1, all are left to a culture in an attempt to form blastocyst embryos. If the patient has 4 or fewer eggs on day 1, the embryos are either transferred on day 3 or frozen for future use. Of course, if a patient is doing preimplantation genetic testing (PGT), we will attempt a blastocyst culture even if the patient has less than 5 fertilized eggs as PGT requires blastocyst embryos.
This approach was originally proposed by Dr. Racowsky and is supported by other highly cited pieces of research
Of course, if a patient has notifies us of a preference other than our standard protocol, we will be happy to follow their wishes.
Conclusion – Day 3 v.s. Day 5 Embryo Transfers
Deciding between day 3 and day 5 embryo transfers can be difficult. Both the good and bad news is that research hasn’t definitely concluded what is best. That’s bad in that the answer to your question, is a “day 5 embryo transfer better than a day 3 embryo transfer” is, “well, maybe,” but good news because nature may have set it up this way. There may not actually be a better embryo type to transfer.
That said, there seems to be enough evidence to support a sound policy. If 4 or more embryos are thriving on day 3, attempt a blastocyst culture. If 3 or fewer embryos are available on day three, transfer or freeze at cleavage.
Of course, it’s always best to discuss all your healthcare plans with your own fertility specialist. Fortunately, you’ll now have all the knowledge you need to make that a highly informed discussion.
If you still have additional questions or if you would like to discuss your fertility treatment options with one of our providers, we encourage you to schedule a consultation.