Intracytoplasmic Sperm Injection (ICSI) in IVF: How the ICSI Procedure Works, Who It Helps, and What to Expect
Intracytoplasmic sperm injection (ICSI) is an advanced lab technique used during IVF to help fertilization occur.
In ICSI, a single sperm is injected directly into a mature egg, bypassing steps that sperm normally must complete to penetrate and fertilize an egg on its own.
ICSI was originally developed to help overcome male factor infertility (such as very low sperm count or low motility), but over time, it has also become widely used in many IVF cycles, including some without clear male factor infertility.
Quick facts: ICSI IVF
What is ICSI in IVF?
ICSI is one of two main fertilization methods used in IVF:
Conventional IVF insemination: many sperm are placed with each egg, and fertilization happens “on its own” if sperm successfully penetrates the egg.
ICSI: a single sperm is injected directly into the egg to achieve fertilization.
A helpful way to think about it is that IVF bypasses the fallopian tubes, while ICSI bypasses several of the final sperm-to-egg steps that can fail in male factor infertility. To learn more about ICSI vs. IVF, click here.
The ICSI procedure: step-by-step (what actually happens in the lab)
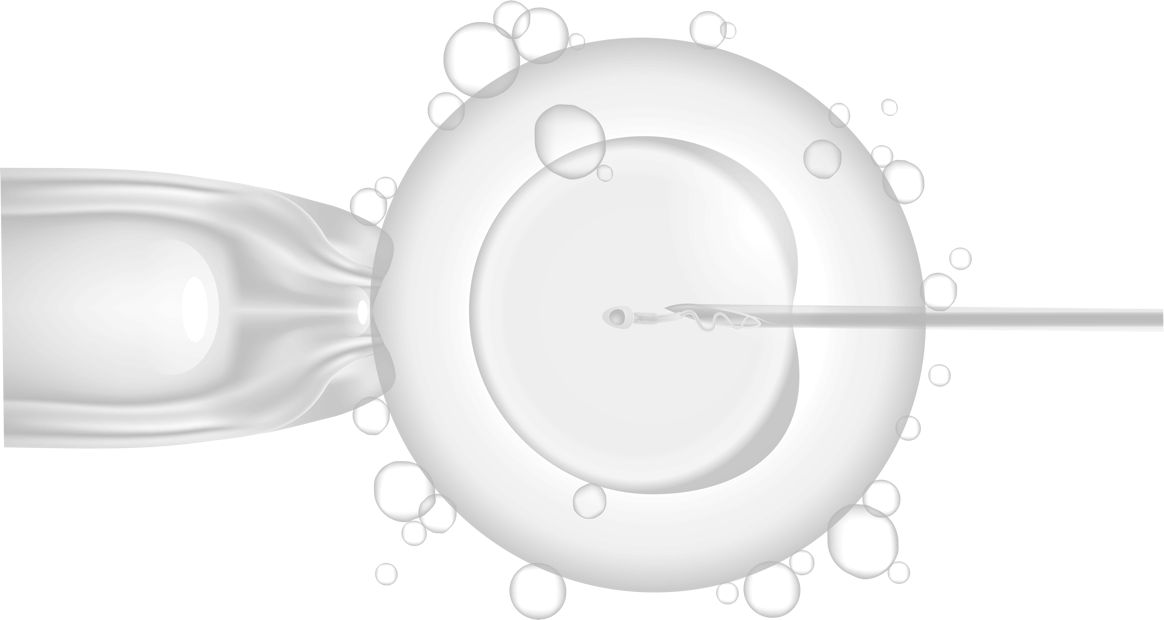
ICSI is performed by an embryologist using micromanipulation tools under a specialized microscope. While exact lab workflows vary, the core steps are consistent:
Egg assessment and preparation (denudation)
Eggs are surrounded by cumulus/granulosa cells. For ICSI, labs typically remove these cells so the embryologist can confirm egg maturity and safely perform injection.Only mature eggs are injected
ICSI is typically performed only on fully mature eggs. In the lab, embryologists often look for a small “polar body” on the egg as a sign that the egg is ready for injection.Sperm selection
The embryologist selects sperm with the best available movement and shape from the processed specimen (or surgically retrieved sperm, depending on the case).Microinjection
Each egg is held steady with a holding pipette while a thin injection needle passes through the zona pellucida and deposits a single sperm into the egg cytoplasm.Fertilization check (the next morning)
Eggs are assessed for normal fertilization (typically, evidence of two pronuclei), and normally fertilized eggs are cultured into embryos for transfer or freezing.
What happens before ICSI?
ICSI is not a separate treatment from IVF. It is one of the fertilization methods used in an IVF cycle.
Most ICSI cycles include:
- Ovarian stimulation with injectable gonadotropins
- Monitoring with ultrasound and bloodwork
- Trigger injection
- Egg retrieval
- Fertilization via ICSI (or conventional insemination)
- Embryo culture
- Embryo transfer or embryo freezing for a later frozen embryo transfer
When is ICSI recommended?
ICSI is most strongly indicated when fertilization is less likely to occur with conventional insemination, especially in male factor infertility.
At-a-glance: common indications for ICSI
Common reasons clinics recommend ICSI
Moderate to severe male factor infertility (low count, low motility, poor morphology)
Surgically retrieved sperm (for example after vasectomy or when sperm retrieval is required)
Prior fertilization failure or very low fertilization in a previous IVF cycle
Use of preimplantation genetic testing (PGT)
Many programs use ICSI to reduce the risk of contamination from extra sperm when performing embryo genetic testing.Previously cryopreserved (frozen) eggs
Egg freezing can be associated with changes to the zona pellucida that reduce conventional IVF fertilization, so ICSI is commonly used to bypass that barrier.
When ICSI is NOT necessary (when conventional IVF may be enough)
ICSI can be essential in the right cases, but it is not automatically “better” for everyone.
In couples without male factor infertility, evidence shows that routine ICSI does not consistently improve clinical pregnancy or live birth compared with conventional IVF insemination.
This is why many fertility teams make the decision based on your semen analysis, prior fertilization history, lab preferences (including PGT workflow), and the specifics of your cycle.
Success rates: ICSI fertilization vs pregnancy outcomes
A common point of confusion is the difference between:
- Fertilization rate (how many eggs fertilize)
- Clinical pregnancy rate
- Live birth rate
ICSI often achieves high fertilization rates, but higher fertilization does not automatically mean higher live birth rates in all patient groups.
Does ICSI guarantee fertilization?
No. Even with a technically perfect injection, fertilization can fail due to sperm decondensation (“open up inside the egg”) problems or egg quality limitations.
Risks and limitations of ICSI
ICSI is widely considered a safe, established IVF laboratory technique, but it has some limitations.
Key limitations (why fertilization can still fail)
Egg activation failure: sometimes the egg does not initiate the intracellular steps needed to fertilize after injection.
Oocyte quality limitations: poor egg quality (often related to age or ovarian factors) can limit survival, fertilization, and embryo development even with ICSI.
Sperm decondensation problems: in some cases, sperm DNA may not properly decondense inside the egg, contributing to abnormal or failed fertilization.
Sperm DNA integrity issues: ICSI can help achieve fertilization when sperm cannot penetrate the egg, but it does not automatically “repair” underlying sperm DNA damage (which can still affect embryo development).
Safety and child outcomes (clinical framing)
The procedure itself is considered safe, and discussions about child outcomes focus on small absolute risks and the possibility that some risks relate to underlying infertility factors (including genetic contributors to male factor infertility) rather than ICSI alone.
ICSI is widely considered a safe, established IVF laboratory technique. Safety discussions usually focus on two areas:
Procedure-related risks to eggs and embryos
Any micromanipulation can stress eggs, and not every injected egg will survive or fertilize, especially when egg quality is poor.Health outcomes in children conceived with ICSI
ASRM notes that major birth defects occur in about 1.5% to 3% of naturally conceived pregnancies and that certain rare conditions have been associated with ICSI, though the absolute risks remain low. ASRM also emphasizes that some risks may relate to underlying infertility factors (including genetic contributors to male factor infertility) rather than ICSI alone.
Cost of ICSI: national ranges vs CNY Fertility
Many clinics bill ICSI as an add-on to IVF. At CNY Fertility, ICSI is included for self-pay patients as part of their comprehensive IVF packages.
| Service | National Average | CNY Fertility | Notes |
|---|---|---|---|
| ICSI | $1,500 | Included | Standard at CNY |
FAQ: ICSI
What is ICSI?
ICSI is a lab fertilization method in IVF where one sperm is injected directly into one mature egg to help fertilization occur.
What is ICSI IVF?
“ICSI IVF” usually means an IVF cycle where ICSI (rather than conventional insemination) is used to fertilize the eggs.
What is the ICSI procedure like?
An embryologist prepares mature eggs, selects sperm, and injects a single sperm into each mature egg using micromanipulation tools under a microscope.
Is ICSI better than IVF?
ICSI is not “better” across the board. It is most helpful when fertilization is unlikely with conventional insemination (especially male factor infertility). In non-male factor infertility, routine ICSI has not consistently improved live birth outcomes over conventional IVF.
ICSI: The takeaway
ICSI is a powerful IVF lab tool that can make fertilization possible when sperm cannot reliably fertilize an egg on its own. It is most clearly beneficial for male factor infertility and prior fertilization failure. For many couples without male factor infertility, ICSI may not improve pregnancy or live birth rates compared with conventional IVF insemination, which is why individualized decision-making with your fertility team matters.