Reproductive Immunology & Inflammation
What is Reproductive Immunology?
Who Should Consider Reproductive Immunology?
- Three miscarriages or IVF failures before the age of 35
- Two miscarriages or IVF failures after the age of 35
- Previous/known immunological problems (rheumatoid arthritis, lupus, positive for antinuclear antibodies, or other immune disorders)
- those with inadequate egg production from a stimulated cycle (number considered inadequate depends on egg and ovarian reserve – best understood in connection with your reproductive endocrinologist)
- previous pregnancies that have shown abnormal fetal growth
- those with one living child and multiple miscarriages while trying to have a second
- A blighted ovum
Reproductive Immunology Testing
It is our opinion that the best tests are those mentioned above, particularly a history of multiple failed IVF cycles or recurrent pregnancy loss. While there are several immunological tests, it’s our general belief that the testing available in today’s age is not fully adequate to identify specific problems. A history of failed IVF or recurrent pregnancy loss is proof enough of a problem. It provides the necessary information on how to treat recurrent failed IVF or recurrent pregnancy loss.
That said, we can take blood and endometrial sample to look at the pathology of the blood and endometrial tissue to determine if there is abundant evidence of inflammation. CNY Fertility offers the latest diagnostic testing and treatment options available for immunological conditions.
Some standard tests for reproductive immunology are as follow:
Antinuclear antibodies (ANA)
An antinuclear antibody test detects antibodies that are reactive to components of the nucleus of a cell (for instance, DNA, Nucleotides, and Histones (both of which are components of DNA), which can leak into the bloodstream following cellular death). Those who test positive (a speckled pattern with a titer 1:40 or higher) for antibodies have been found to have a higher risk for recurrent pregnancy loss.
Antiphospholipid Antibody (APA)
Phospholipids are an important group of molecules found on the surface of cells. While most cells only displace these cellular structures on occasion, placental cells always have phospholipids present in their cell membrane. High levels of APAs that “attack” these phospholipids increase blood coagulation and thus the restriction of blood flow. The lack of blood from this thickening to an early-stage embryo or fetus through placental tissue (which is involved in nutrient and oxygen exchange with the fetus), can lead to fetal demise,
Antithyroid Antibodies (ATA)
ATAs are associated with an increase in pro-inflammatory cytokines secreted by T cells in the uterine lining. As such, elevated ATAs may represent underlying T cell dysfunction affecting implantation.
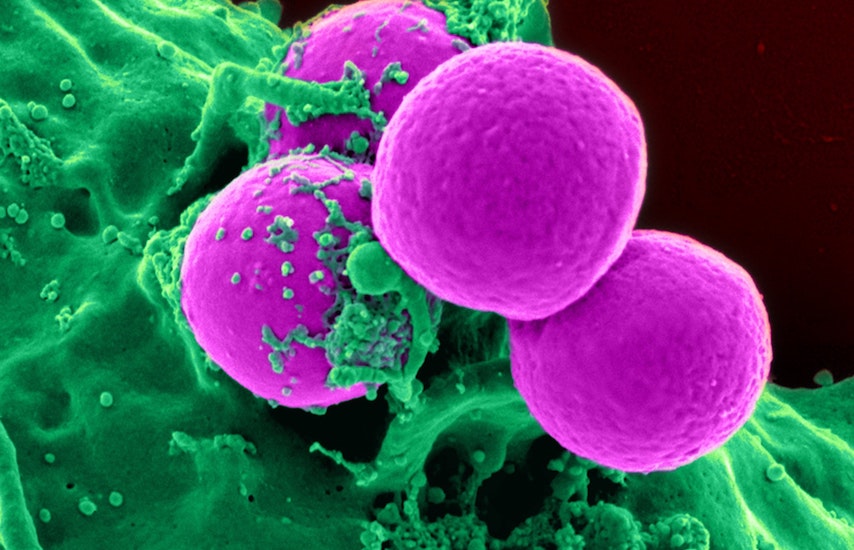
Natural Killer Cell Assay
Natural Killer Cells are a type of white blood cell that perform many essential functions including cellular surveillance for infections and cancerous cells. Elevated levels of circulating NK cells are associated with recurrent pregnancy loss. A Natural Killer Assay looks for circulating natural killer (NK) cell activity as well as the ability of immunoglobulins’ ability to suppress that activity.
Helper T 1 & 2 Assay
Helper T-cells are a type of lymphocyte that can be further divided into Helper 1 and 2 cells. Helper 1 cells secrete cytokines that direct immune cells to attack and kill cells that they think are infected or abnormal. Helper 2 cells secrete cytokines that counteract those secreted by Helper 1 cells. There is a natural balance between this system, but those with higher ratios often have higher levels of infertility and pregnancy loss.
Regulatory T Cells
Regulatory T cells are thought to play an essential role in controlling the natural tendency of a woman’s immune system to reject a semi-foreign fetus (remember, a fetus is made up of different DNA than the mother). Higher numbers of regulatory T-Cells in blood and endometrial lining have been associated with better pregnancy outcomes.
Reproductive Immunophenotype
A reproductive immunophenotype looks at the percentage of lymphocyte types in the blood, including CD-3, CD-4, CD-8, CD-19, CD-5, CD56, CD16.
Thrombophilias
Thrombophilias is an increased tendency for blood to clot. During healthy pregnancy, the mother’s ability to produce blood clots in the uterus and the placenta is suppressed. Certain conditions may prevent the normal suppression of this clotting, which could result in pregnancy complications and fetal demise.
What Causes Immunologically Related Inflammation and Infertility?
We believe that diet is the number one source of chronic inflammation and fertility dysfunction. The Standard American Diet is a carbohydrate-rich diet that causes chronic hyperglycemia leading to systemic inflammation compounded by a constant bombardment of plant antigens and bacterial overload from plants. We recommend those dealing with infertility to practice a high fat low carbohydrate diet for fertility.
Reproductive Immunology Treatment
Recently, we have achieved success in treating inflammation pharmacologically with low-dose steroids like Prednisone, Humira, intravenous immunoglobulins, and intralipids. The fat appears to be a successful method of reducing inflammation in our bodies. Our oocyte enhancement and implantation enhancement protocols, in conjunction with our standard protocols, provide our clients with the very best opportunity for a successful pregnancy.
However, since the source of inflammation is likely related to the food we eat, it only makes sense that making dietary changes and supplements that can and will reduce inflammation. There is ample evidence that excessive amounts of carbohydrates, sugars, grains, fruits, fiber, and vegetables along with milk products are very inflammatory to our bodies and increase the number of antigen/antibody interactions. These white cells and cytokines that are enhanced in our bodies, in many cases, are not specific to a particular area. You might feel it in your joints, your skin, bowel, head, eyes, or you may not even feel it at all. But, you have a problem that results in repetitive pregnancy loss, failed implantation from IUI, IVF or natural cycles, or simply not conceiving.