ICSI: What is ICSI IVF?
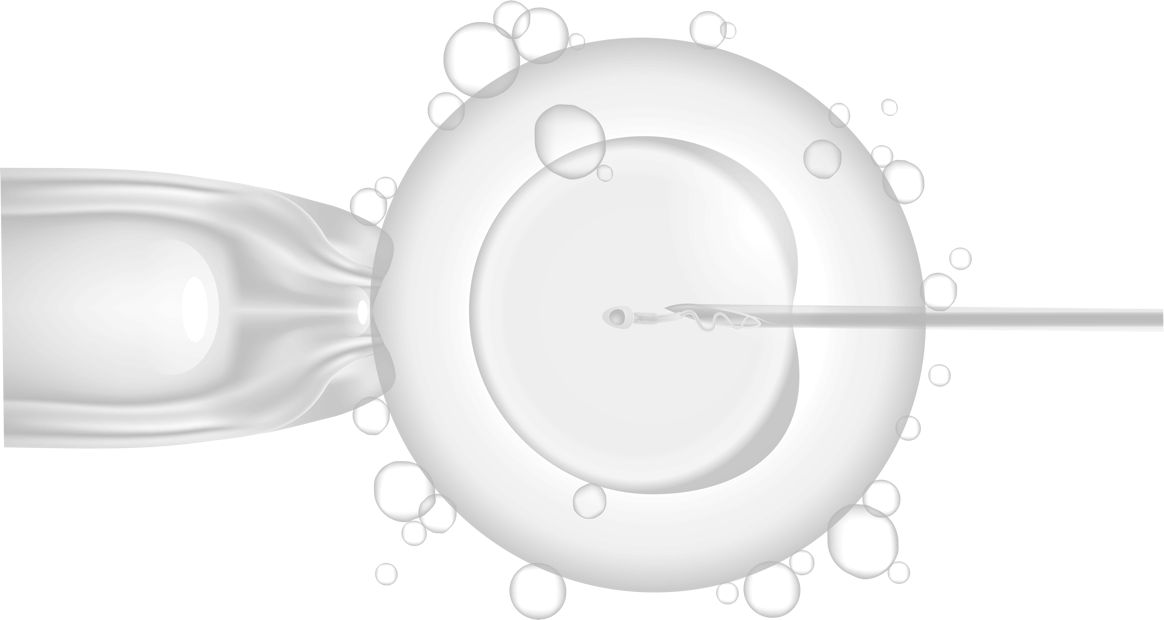
Intracytoplasmic Sperm Injection (ICSI) [pronounced “ick-see”] is an advanced reproductive procedure done in an embryology lab during an IVF treatment in which a single sperm is injected directly into a woman’s egg in order to create a fertilized embryo. ICSI IVF is one of two fertilization methods that can be used during IVF, the other being Conventional IVF Fertilization.
The ICSI Procedure
During ICSI, an embryologist identifies and uses what appear to be the best sperm to directly inject into the egg. Sperm are selected by looking at the morphology (shape) and progression (forward movement). The sperm are then aspirated from the sperm drop into a microtool called an ICSI needle. Once the sperm is in the ICSI needle, the embryologist moves it to a media drop containing the eggs. The egg to be injected is held gently in place by a microtool called a holding pipette, which exerts a light suction on the egg, allowing the embryologist to place the egg in perfect injection position. The embryologist then brings the ICSI needle with the sperm down to the other media drop and lines it up with the egg. The ICSI needle is gently pressed into the side of the egg below the polar body. The zona pellucida and oolemma (membrane between the egg’s innards and the zona pellucida) are punctured and a small part of the ooplasm is aspirated into the needle to gently mix it before the sperm is placed into the egg. Embryologists typically combine several pairs of egg and sperm depending on how many eggs were retrieved during that cycle.
What eggs are injected?
Only mature eggs are injected via ICSI, and not all retrieved eggs reach maturity. The polar body indicates that the egg is mature and ready for insemination. Eggs must have all of the protective granulosa cells removed prior to ICSI so that the polar body can be visualized. This process was initially developed for men whose sperm had low motility, and could not penetrate the zona pellucida.
What happens before ICSI?
The process that leads up to the insemination of eggs with sperm is called controlled ovarian hyperstimulation. This is when a woman’s ovaries are hyperstimulated to produce multiple follicles, each potentially containing an egg. Ovarian hyperstimulation is achieved by a woman taking gonadotropins (injectables Follistim and Gonal-F) while monitoring the response/follicular growth to the medication.
Once the eggs have been retrieved during an in-office procedure called an egg (oocyte) retrieval, it is time for the true IVF to begin. Eggs can be fertilized via ICSI or conventional insemination.
ICSI vs. IVF: What’s the difference between ICSI and Conventional IVF Fertilization
Both ICSI and conventional IVF are subtypes of IVF. Conventional IVF was developed to circumvent female fertility problems such as blockages in the Fallopian tubes, endometriosis, or when previous IUI cycles were not successful. If using conventional fertilization, eggs are placed in media drops and sperm is then added to those drops. This allows the sperm to penetrate the egg’s zona pellucida (outside shell) and deposit the male’s DNA into the egg’s ooplasm (egg’s cytoplasmic matrix), hopefully resulting in fertilization of the egg.
ICSI is a more recent technology developed with male factor infertility in mind, allowing men with low sperm count (oligozoospermia) or immotile sperm (asthenozoospermia) to father a child. During traditional IVF, many sperm are placed together with an egg in hopes that one of the sperm will enter and fertilize the egg on its own. With ICSI, the embryologist takes a single sperm and injects it directly into an egg. Today ICSI is widely used in fertility clinics and is typically the method of choice even in cases where male infertility isn’t a factor.
The ICSI technique fertilizes on average 50-80% of the eggs that are injected, whereas conventional IVF fertilizes around 50% of eggs. But fertilization rates are different than clinical pregnancy or live birth rates. After fertilization occurs, success rates for couples using ICSI with IVF are the same as for a couple using regular IVF treatment.
ICSI has the ability to achieve good reproductive outcomes in cases where traditional IVF would not, however in cases where male infertility is not an issue, multiple studies have demonstrated fertilization and pregnancy success rates with ICSI are equivalent to standard insemination by IVF. ICSI has not yet been shown to be more effective than IVF without ICSI in patients without male factor infertility.
The success rates of each method are highly dependent on the skill of the embryologist, egg and sperm quality, and the overall health and causes of infertility in both partners. All things being equal, one method is not better than the other. The choice of ICSI or traditional IVF is highly dependent on the specifics of each individual case. If there are a limited number of eggs, ICSI often preferred because it optimizes the odds as the highest quality sperm are selected. When donor sperm or eggs are used, ICSI is often considered unnecessary because the quality of both gametes is so high.
Whether you opt for ICSI or conventional IVF, the ovarian stimulation and egg retrieval process remains the same, only the fertilization process itself is different. With both techniques, the eggs are checked the morning after to determine whether fertilization has occurred.
After the eggs are determined to be fertilized, they are called embryos. The embryos are in special petri dishes for the next 2-6 days, allowing cells to divide and grow. Once the embryos reach the proper growth stage, they are transferred back to the female patient’s uterus to establish a pregnancy.
At CNY Fertility, ICSI is used in 99% of cases because it reduces the risk of fertilization failure due to the sperm’s inability to penetrate the egg. However, both techniques are available to our patients.
WHY Choose ICSI?
If male factor infertility is a concern (usually identified with a semen analysis), ICSI can be the perfect solution. Using ICSI effectively eliminates male infertility by inserting sperm cells directly into the egg. Sperm count, motility, and morphology all play vital roles in male fertility and are crucial to sperm successfully meeting and penetrating the egg during natural conception. With ICSI, there’s no hoping a few powerful, healthy sperm make the perilous journey from the man’s epididymis through the vagina, cervix, uterus, and fallopian tubes to eventually find the egg; it’s guaranteed. ICSI can also be a great solution to an irreversible vasectomy or for men suffering from paralysis.
Male factor infertility isn’t the only reason for choosing ICSI. Your reproductive endocrinologist may recommend ICSI for other reasons including:
- If previous IVF cycles produced few or no fertilized eggs;
- If using frozen sperm and thawed sperm don’t appear active;
- If using frozen eggs – the process of vitrification can sometimes harden the egg’s outer shell making fertilization challenging;
- If doing Preimplantation Genetic Testing (PGT), ICSI is generally recommended because additional sperm near the embryo can interfere with results.
- To simply achieve a higher chance of fertilization.
Does ICSI Guarantee Fertilization?
Some people wrongly assume that ICSI guarantees fertilization. While ICSI greatly improves the likelihood of fertilization, it does not guarantee it. The ICSI procedure fertilizes 50 to 80 percent of eggs, but results vary depending on maternal age, egg quality, and sperm quality.
Since ICSI sounds like a sure thing, many people wonder what would prevent fertilization from occurring. Assuming there is not a technical reason for the failure, there are a couple factors that may explain why fertilization doesn’t happen:
- The egg may not have survived after the injection of sperm. This can happen if the eggs are post-mature or if they matured just prior to ICSI. Poor egg quality can also be a factor in the failure to fertilize.
- The sperm head may not have decondensed. If the DNA of the sperm remain locked in the sperm head then fertilization fails to occur or there is abnormal fertilization.
- The egg may not have been activated and didn’t participate in the intracellular steps of fertilization. This is a common reason for fertilization failure after ICSI.
Is ICSI Safe?
The procedure itself is very safe and has the same risks as regular IVF. But questions often arise regarding the safety of ICSI for the offspring produced as a result of its use. The American Society of Reproductive Medicine states that “If a woman gets pregnant naturally, there is a 1.5% to 3% chance that the baby will have a major birth defect. The chance of birth defects after ICSI are rare. Certain conditions that have been associated with the use of ICSI (Beckwith-Wiedemann syndrome, Angelman syndrome, hypospadias, or sex chromosome abnormalities) are thought to occur in far less than 1% of children conceived using this technique. Some of the problems that cause a patient’s infertility may be genetic (their fathers have male factor infertility). Therefore, boys (of men with male factor fertility) conceived with the use of ICSI may have infertility issues as adults.”
Cost of ICSI: National Average Compared to CNY Fertility
ICSI is an innovative option for family building, giving many couples the potential for genetically-related children that did not exist before its development.
Some fertility clinics consider ICSI to be an additional procedure above and beyond conventional IVF adding anywhere from $800-2,500 to the total cost of IVF depending on where you live around the country. At CNY Fertility, ICSI (along with assisted hatching) is included with IVF for all self-pay patients.
Here at CNY, our IVF (conventional or ICSI fertilization) starts at just $4,250 per cycle—less than a third of the national average.
For more information about ICSI and Conventional IVF, feel free to schedule a consultation.