Diminished Ovarian Reserve: Symptoms, Causes, and How It Affects Fertility
Diminished ovarian reserve (DOR) is a fertility diagnosis that means the ovaries contain fewer eggs than expected for a person’s age, and that egg quality may also be reduced. DOR is common, especially in women in their 30s and 40s, though it can occur earlier.
Understanding what diminished ovarian reserve means, why it happens, and how it affects fertility can help you make informed decisions about next steps.
This guide explains what DOR is, how it is diagnosed, what causes it, and the treatment options available.
Quick Facts About Diminished Ovarian Reserve
• DOR refers to reduced egg quantity and often reduced egg quality for age
• Egg number declines continuously and cannot be replenished
• Many people with DOR have no symptoms
• Ovarian reserve tests predict response to stimulation, not natural fertility
• Age remains the strongest predictor of pregnancy and live birth
What Is Diminished Ovarian Reserve?
Diminished ovarian reserve means that the ovaries contain fewer eggs than expected for age, and that remaining eggs may have reduced developmental potential.
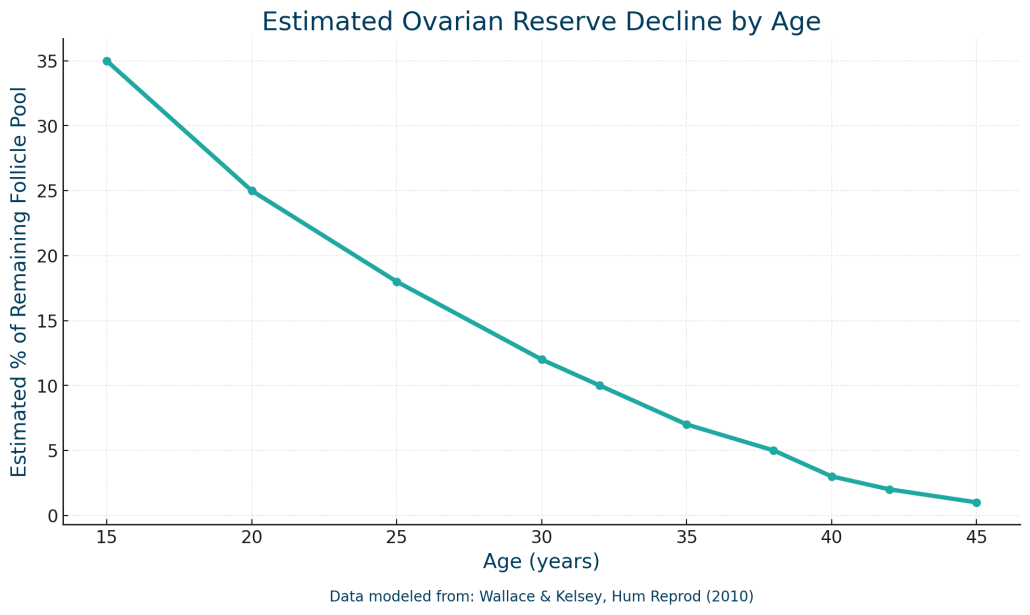
Women are born with a finite number of follicles. Each follicle contains an immature egg. Over time, follicles are lost through a natural process of ovarian aging and cannot be replaced.
Scientific reviews show that ovarian aging involves both loss of egg number and decline in egg quality, with an accelerated decline beginning in the mid-30s.
How Is Diminished Ovarian Reserve Diagnosed?
DOR is diagnosed using a combination of ovarian reserve tests. These tests help estimate how the ovaries may respond to fertility medications rather than predicting natural conception.
Common Ovarian Reserve Tests
| Test | What It Measures | What It Predicts |
|---|---|---|
| AMH | Hormone produced by growing follicles | Expected ovarian response |
| AFC | Small resting follicles on ultrasound | Number of recruitable follicles |
| FSH | Pituitary hormone measured early cycle | Ovarian feedback and reserve |
Research shows that antral follicle count (AFC) is one of the strongest predictors of ovarian response to stimulation, while age remains the strongest predictor of live birth.
Symptoms of Diminished Ovarian Reserve
Many individuals with diminished ovarian reserve feel completely healthy and only discover DOR through fertility testing.
Possible findings include:
• Low AMH for age
• Fewer antral follicles on ultrasound
• Higher early-cycle FSH or estradiol
• Shorter menstrual cycles
• Reduced response to fertility medications
• Difficulty conceiving after 6 to 12 months
Clinical reviews emphasize that ovarian reserve decline often occurs silently and is best assessed with hormone testing and ultrasound rather than symptoms alone.
What Causes Diminished Ovarian Reserve?
DOR can have multiple contributing factors, and sometimes no clear cause is identified.
Age
Age is the most significant contributor to ovarian reserve decline. Egg number and quality decrease steadily over time, with an accelerated decline beginning in the mid-30s.
Genetic Factors
Some individuals are born with fewer follicles or experience faster follicle loss due to genetic influences.
Autoimmune and Endocrine Conditions
Autoimmune disorders and endocrine conditions such as thyroid disease have been associated with reduced ovarian reserve.
Surgery, Chemotherapy, or Radiation
Ovarian surgery, chemotherapy, and pelvic radiation can reduce ovarian reserve.
Environmental Toxins
Associations have been observed between reduced ovarian reserve and exposure to endocrine-disrupting chemicals such as BPA and certain pesticides.
These studies describe associations rather than proven cause and effect.
Endometriosis
Endometriosis, particularly ovarian endometriomas and their surgical removal, is strongly linked to reduced ovarian reserve.
Can Diminished Ovarian Reserve Be Reversed?
Egg quantity cannot be restored. However, some strategies may help optimize egg quality and ovarian response.
Evidence-Based Support Strategies
CoQ10
Randomized controlled trials show improved ovarian response and embryo quality with CoQ10 pretreatment.
Vitamin D
Meta-analysis suggests higher live birth rates among vitamin D-replete women undergoing assisted reproduction.
Omega-3 Fatty Acids
Emerging data suggest potential ovarian protective effects, though human evidence remains limited.
Experimental Approaches
Intra-ovarian PRP
PRP has shown potential improvements in ovarian reserve markers, but evidence remains limited and experimental.
Can You Get Pregnant With Diminished Ovarian Reserve?
Yes. Many individuals with DOR conceive naturally or with treatment, though average success rates per cycle are lower.
Studies show pregnancy and live birth are still achievable, especially in younger patients and across multiple IVF cycles.
Age remains the strongest predictor of outcomes.
Treatment Options for Diminished Ovarian Reserve
| Option | When It May Be Used |
|---|---|
| Timed intercourse or IUI | Younger patients with mild DOR |
| Conventional IVF | Tailored stimulation protocols |
| Mini or modified natural IVF | Very low follicle response |
| Donor egg IVF | Severe DOR or advanced age |
| Supportive strategies | Supplements and experimental approaches |
Ovarian reserve tests guide individualized treatment planning.
When Should You Get Tested?
Fertility evaluation is recommended based on ASRM guidance.
Earlier testing may be appropriate with endometriosis, cycle changes, family history of early menopause, prior ovarian surgery, or when considering fertility preservation.
Diminished Ovarian Reserve: The Takeaway
Diminished ovarian reserve does not mean your fertility journey is over. While egg quantity cannot be restored, many people with DOR go on to conceive.
Understanding your ovarian reserve in context, optimizing egg quality where possible, and choosing evidence-based treatment strategies can help you move forward.
At CNY Fertility, we work with many individuals who have low AMH, low AFC, high FSH, or past poor response to stimulation. Schedule a consultation to learn how our team can help you interpret your results, explore options, and design a plan that balances the science with your personal and financial realities.

