Day 3 v.s. Day 5 Embryo Transfer
One of the most debated questions in IVF is whether to transfer embryos at the cleavage stage (day 3) or blastocyst stage (day 5–7).
As lab technologies have advanced, day 5 transfers have become increasingly common, and the American Society for Reproductive Medicine generally recommends a blastocyst transfer for patients with a good prognosis of success.
However, not all patients fall into this category. Extending embryo development in the lab carries risks, and research has yet to reach a clear consensus on whether day 3 or day 5 transfers offer better outcomes.
In this article, we’ll explore embryo development, the arguments for each approach, success rates, and how we at CNY Fertility determine the optimal timing for transfer.
Day 3 vs. Day 5 Embryo Fast Facts
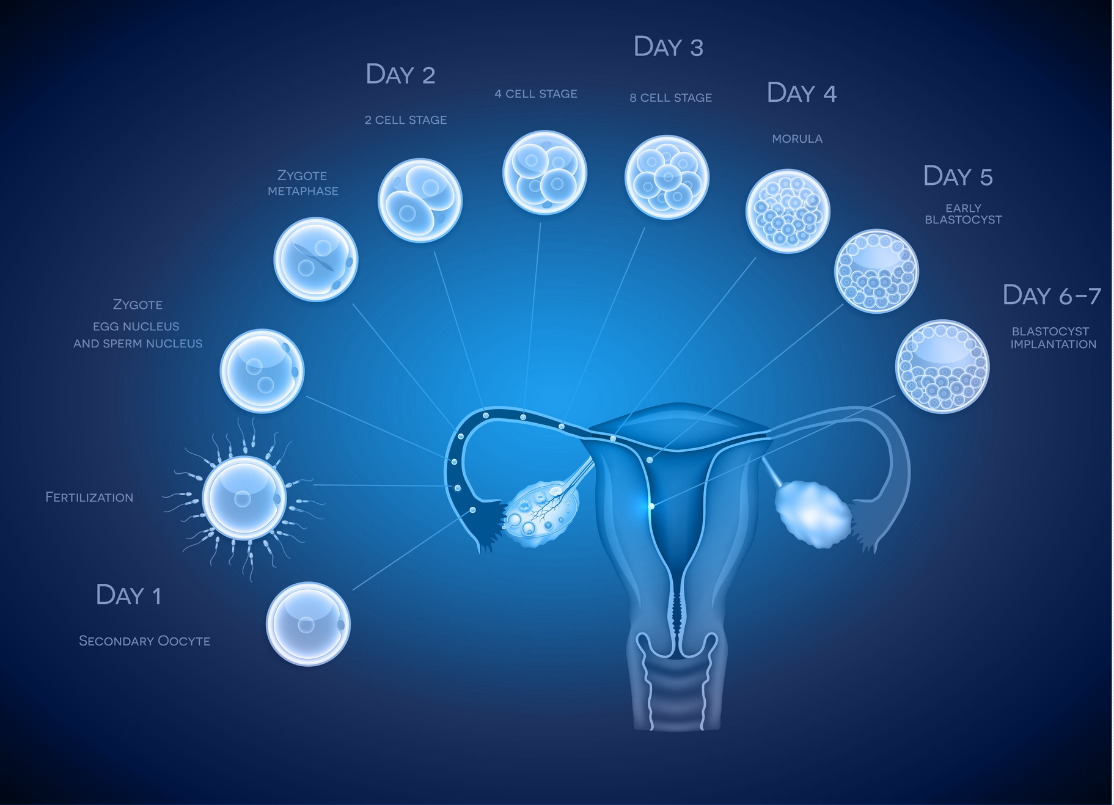
An embryo begins as a single cell. By day 3, it usually develops into a 6–8 cell “cleavage-stage” embryo. By day 5–7, it may reach the blastocyst stage.
There is attrition at every stage of development. For example, 10 embryos on the day of fertilization may decrease to 5 embryos by day 3, and only 2 by day 5. Some patients may not produce any day 5 embryos, even after multiple IVF cycles.
Because of this attrition, patients typically have more embryos available for transfer on day 3 than on day 5.
Blastocyst-stage embryos tend to have higher implantation rates, likely because they are more developed and have a greater chance of being chromosomally normal.
Despite these higher implantation rates, cleavage and blastocyst-stage embryos have similar pregnancy and live birth outcomes on a per-retrieval basis. This is because more embryos are available on day 3, which increases the likelihood of having multiple transfers if the first attempt fails.
Both day 3 and day 5 transfers are supported by scientific evidence, and each has advantages depending on the patient’s circumstances.
At CNY Fertility, our approach is tailored: if a patient has 5 or more fertilized eggs on day 1, blastocyst culture is attempted. If there are 4 or fewer embryos, they are usually transferred or frozen on day 3, unless preimplantation genetic testing (PGT) is planned.
Introduction to the Arguments for Both Day 3 and Day 5 Embryo Transfer
There is strong scientific evidence supporting both day 3 and day 5 embryo transfers. The debate between the two generally centers on the following arguments:
Day 5
Blastocyst (day 5) embryos are more mature and have already demonstrated a higher likelihood of being chromosomally normal, since weaker embryos typically stop developing before this stage.
If an embryo has the genetic makeup and “strength” to survive 5 days in the lab, it may have a better chance of resulting in pregnancy once transferred.
As a result, fewer embryos usually need to be transferred, maintaining higher success rates while reducing the risk of twins or higher-order multiples.
Day 5 transfers also align more closely with natural biology because implantation after intercourse typically occurs between days 5–7.
Day 5 embryos can be biopsied for genetic testing, though there is ongoing debate about the accuracy, timing, and necessity of this practice.
Day 3
Even the most advanced lab cannot fully replicate the uterine environment. Embryos that reach day 3 have already proven their genetic viability and resilience, making them candidates for transfer.
Some day 3 embryos that might thrive in the uterus could fail to survive if kept in the lab until day 5, meaning viable embryos could be lost before they are ever given the chance to implant.
Despite some stigma around day 3 transfers, research shows that live birth rates per IVF retrieval can be equal, or in some cases higher, than with day 5 transfers.
Ultimately, many fertility doctors and clinics, including CNY Fertility, use both approaches depending on each individual case. There is no absolute “right” or “wrong” choice, only the protocol that’s best suited to the patient’s unique circumstances.
Day 3 “Cleavage Stage” Embryos Explained
By day 3, most embryos have undergone several rounds of cell division and typically contain 6 to 10 cells, though some may have as few as 4. At this stage, they are called cleavage-stage embryos, since the cells are dividing, but the overall size of the embryo has not yet increased.
Large-scale studies suggest that embryos with 8 or more cells on day 3 are associated with significantly higher live birth rates compared to those with fewer cells.
Day 5 “Blastocyst Stage” Embryos Explained
By day 5, embryos typically reach the blastocyst stage of development.
At this point, cell division accelerates, and the cells begin to specialize into two distinct groups: the inner cell mass, which develops into the fetus, and the trophectoderm epithelium, which forms the placenta and other tissues needed to support pregnancy.
Allowing embryos to grow to the blastocyst stage can serve as an important selection tool, since healthier embryos are more likely to progress to this stage and, therefore, may have a higher chance of successful implantation and pregnancy.
Success Rate Comparison
Extending embryo growth to day 5 may help embryologists select stronger embryos and improve synchrony with the uterine lining, but does it make a real difference?
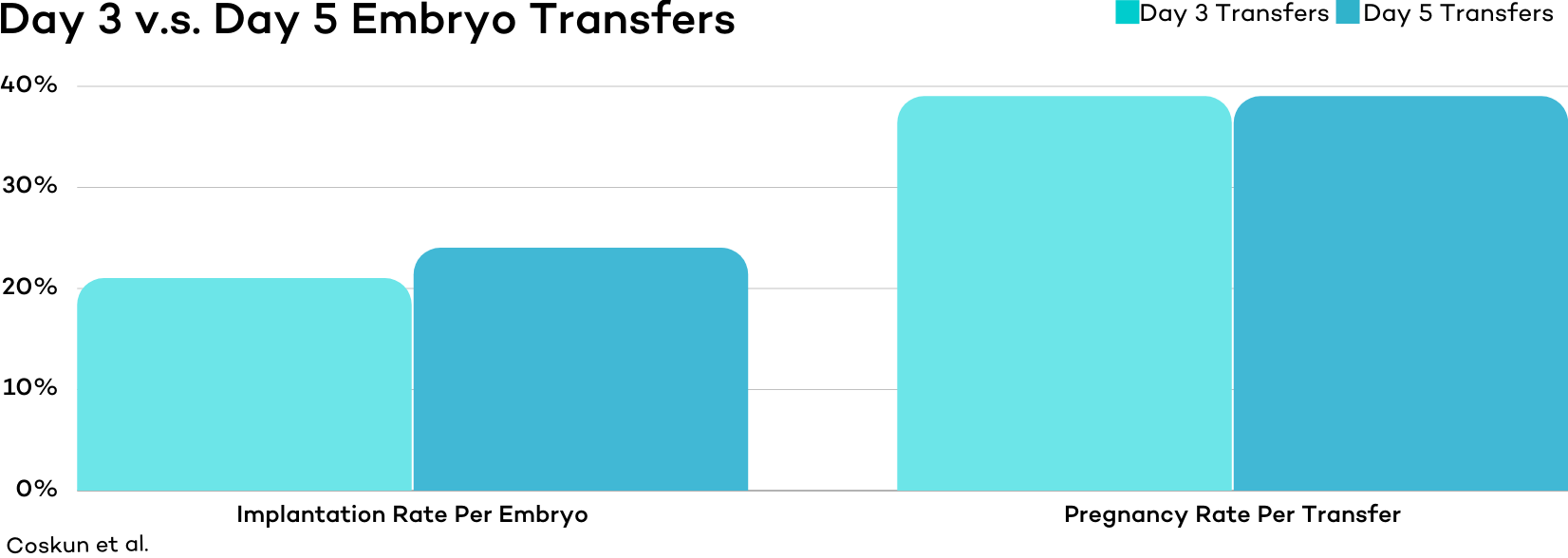
A randomized trial published in Human Reproduction in 2000 assigned 201 women to either day 3 or day 5 transfer groups, with 2–3 of the best-graded embryos transferred per patient.
Implantation rates per embryo were slightly higher in the day 5 group (24%) compared to the day 3 group (21%).
However, because slightly more embryos were transferred in the day 3 group, overall pregnancy rates were identical at 39% for both groups.
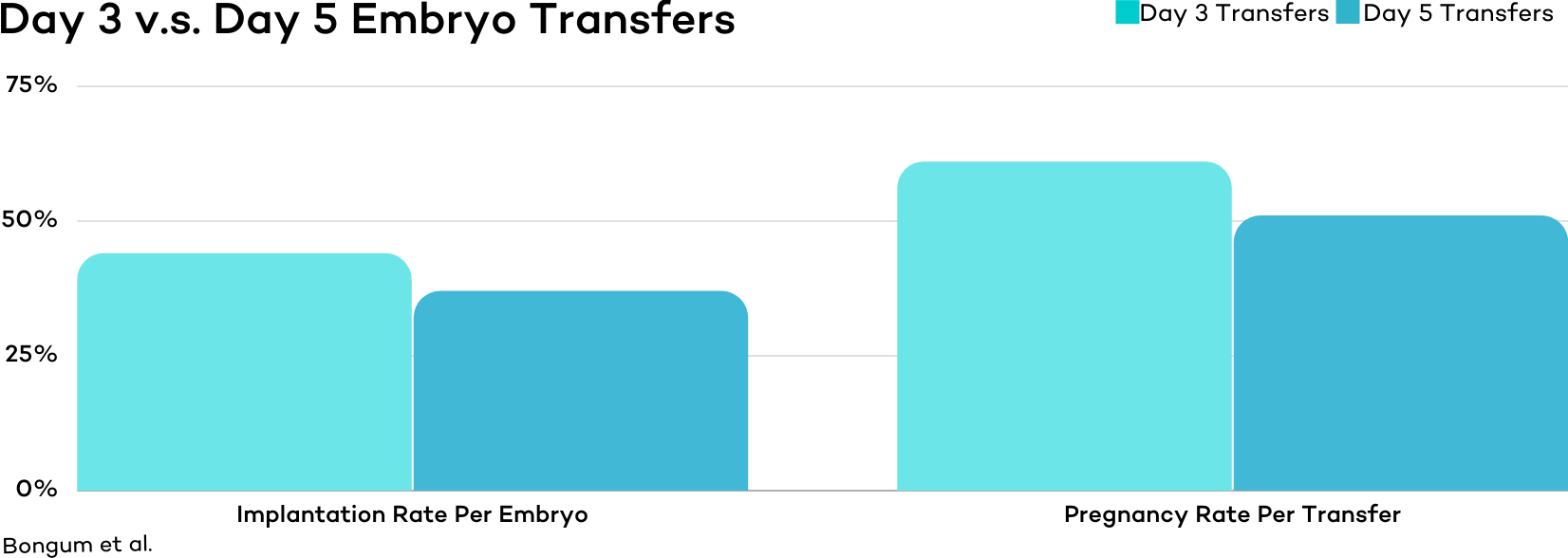
Although differences in results were statistically insignificant, another study published in 2003 from Denmark found that Day 3 Embryos (with at least 8 cells) have slightly better outcomes compared to blastocyst embryos.
In this study, implantation rates were 44% for day 3 embryos versus 37% for blastocysts, and clinical pregnancy rates were 61% for day 3 embryos versus 51% for blastocysts.
Another randomized controlled trial published in 2017 reached similar conclusions. In this study, 190 women were assigned to either day 3 or day 5 transfer groups, and the outcomes showed no significant difference between the two approaches.
Measure | Day 3 Transfers | Day 5 Transfers |
Implantation Rate | 47.4% | 45.3% |
Clinical Pregnancies | 46.3% | 44.2% |
Live Births | 36.8% | 34.7% |
Interestingly, one of the most frequently cited studies on this topic–often referenced by ASRM to support the preferential transfer of blastocyst embryos–did not find a statistically significant difference in pregnancy rates between day 3 and day 5 transfers (66% vs. 71%).
However, that study did show a significant difference in implantation rates, 30% for day 3 versus 50% for day 5.
In other words, to achieve comparable pregnancy rates, more embryos were transferred at the cleavage stage. One positive takeaway is that on day 3, there are typically more embryos available, so transferring additional embryos is often feasible.
Day of Transfer | Day 3 Cleavage | Day 5 Blastocyst |
Number of Embryos Transferred | 2.2 | 3.7 |
Implantation Rate | 30% | 50% |
Clinical Pregnancy Rate | 66% | 71% |
That being said, other studies point to the advantages of day 5 transfers.
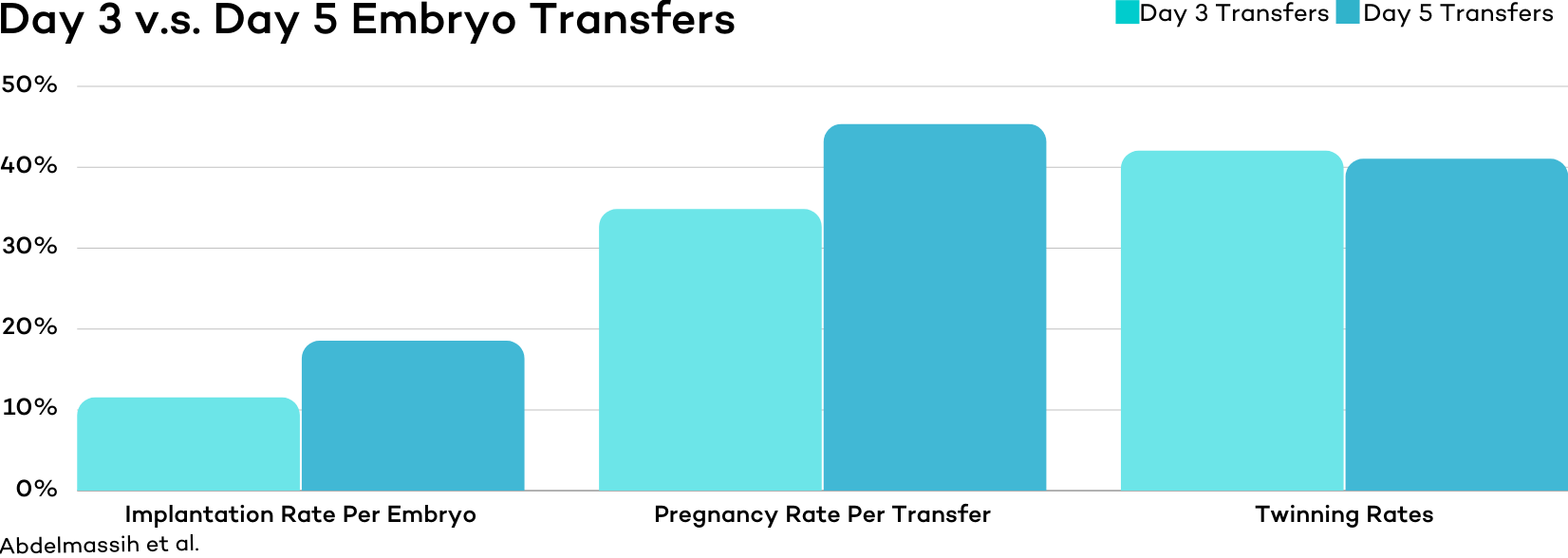
One study conducted at a private fertility clinic found that patients in the day 5 transfer group experienced higher implantation and pregnancy rates, along with lower rates of multiple gestations.
Pregnancy rates were 34.8% for day 3 embryos versus 45.3% for blastocysts, implantation rates were 11.5% versus 18.5%, and multiple gestation rates were 47.1% versus 28.5%.
Another study published in Fertility and Sterility in 2008 found a modest advantage for day 5 embryos when transferring just one of either type of embryo.
Measure | Day 3 | Day 5 |
Clinical Pregnancy | 44% | 52% |
Another often-cited article published in the New England Journal of Medicine evaluated 351 infertile women under the age of 36. Researchers found a significant advantage for blastocyst transfers, with pregnancy rates of 32.0 percent compared to 21.6 percent for cleavage-stage transfers.
In other words, credible evidence exists on both sides of the debate.
In 2016, a large-scale meta-analysis reviewed 27 controlled studies involving 4,031 couples and helped provide greater clarity.
The researchers found that IVF transfers done at the blastocyst stage were more likely to result in pregnancy and birth than transfers done earlier at the cleavage stage. But they caution that the strength of the evidence isn’t very strong.
When evaluating cumulative pregnancy rates across all transfers from a single retrieval, there was no difference between the two groups, though the evidence for this outcome was also very weak.
In other words, while blastocyst transfers may offer some per-transfer advantages, cumulative live birth outcomes appear to be similar when multiple transfers from one retrieval are considered.
The Advantages and Disadvantages of Day 3 Embryo Transfers
Advantages
- Greater number of embryos available for transfer, though a larger proportion may be genetically abnormal
- Embryos are placed in the uterine environment earlier, which may be more natural for development
- Lower risk of cycle cancellation since embryos are transferred before the possibility of lab arrest on day 5
- Comparable live birth rates to later-stage transfers
Disadvantages
- Lower implantation rates per transferred embryo, though more embryos are usually available for transfer on day 3 compared to day 5
- Higher chance of twin or higher-order pregnancies, since more embryos may need to be transferred at once to achieve comparable success rates
- Less detailed information is available from embryo grading, making it harder to assess embryo quality
- Genetic testing cannot be performed on cleavage-stage embryos
The Advantages and Disadvantages of Day 5 Embryo Transfers
Advantages
- Embryos that do not progress to the blastocyst stage are naturally ruled out
- Higher-quality embryos can be identified, allowing fewer embryos to be transferred at once
- Higher implantation rates compared to day 3 transfers
- Usually, fewer total embryo transfers are needed to achieve a live birth
- Preimplantation genetic testing (PGT) can be performed at this stage
Disadvantages
- Higher chance that embryos will not survive to day 5, leaving fewer or no embryos available for transfer
- Greater risk of cycle cancellation
- Embryos are placed into the uterine environment later than in day 3 transfers
- Some viable day 3 embryos may fail to progress to day 5, eliminating potentially healthy options
- Not suitable for patients who produce few embryos
- Some individuals may not be able to develop embryos to the blastocyst stage
The CNY Way
As the mixed data in this article show, even well-controlled randomized studies struggle to determine whether day 3 or day 5 embryo transfers lead to superior live birth rates.
The general consensus, however, is that day 5 transfers offer slightly higher live birth rates per transfer
Yet not all patients can produce blastocyst embryos. For some, attempting to culture embryos to day 5 may result in no embryos available for transfer, and therefore no chance of pregnancy in that cycle.
Because of this, it is important to have a clear system for determining when embryos should be transferred or frozen on day 3 versus when to allow them to develop further.
At CNY Fertility, our approach is based on the number of viable embryos available early in development. If a patient has 5 or more fertilized eggs on day 1, all embryos are typically cultured in an attempt to reach the blastocyst stage. If a patient has 4 or fewer, embryos are usually transferred or frozen on day 3. An exception is made for patients pursuing preimplantation genetic testing (PGT), which requires blastocyst-stage embryos In these cases, we attempt blastocyst culture regardless of the starting number of fertilized eggs.
This method was first proposed by Dr. Racowsky, and has since been supported by other influential studies.
Of course, if a patient has a preference outside of this protocol, we will honor their wishes.
Day 3 vs. Day 5 Embryo Transfers: The Takeaway
Deciding between day 3 and day 5 embryo transfers is not always straightforward. The reality is that research has not definitively concluded which approach is universally better. That may feel frustrating, but it also reflects the fact that both options can lead to healthy pregnancies, and there may not be a single “best” answer for everyone.
The evidence suggests a straightforward guideline: if 4 or more embryos are thriving on day 3, a blastocyst culture is worth pursuing. If 3 or fewer are available on day 3, transferring or freezing at the cleavage stage is generally the wiser choice.
Ultimately, every patient’s situation is unique. It is always best to review your options with your fertility specialist and make the decision that aligns with your individual circumstances. With this shared knowledge, you’ll be well-prepared to have informed and meaningful conversations.