Artificial Insemination: Types, Process, Costs and more
What is Artificial Insemination?
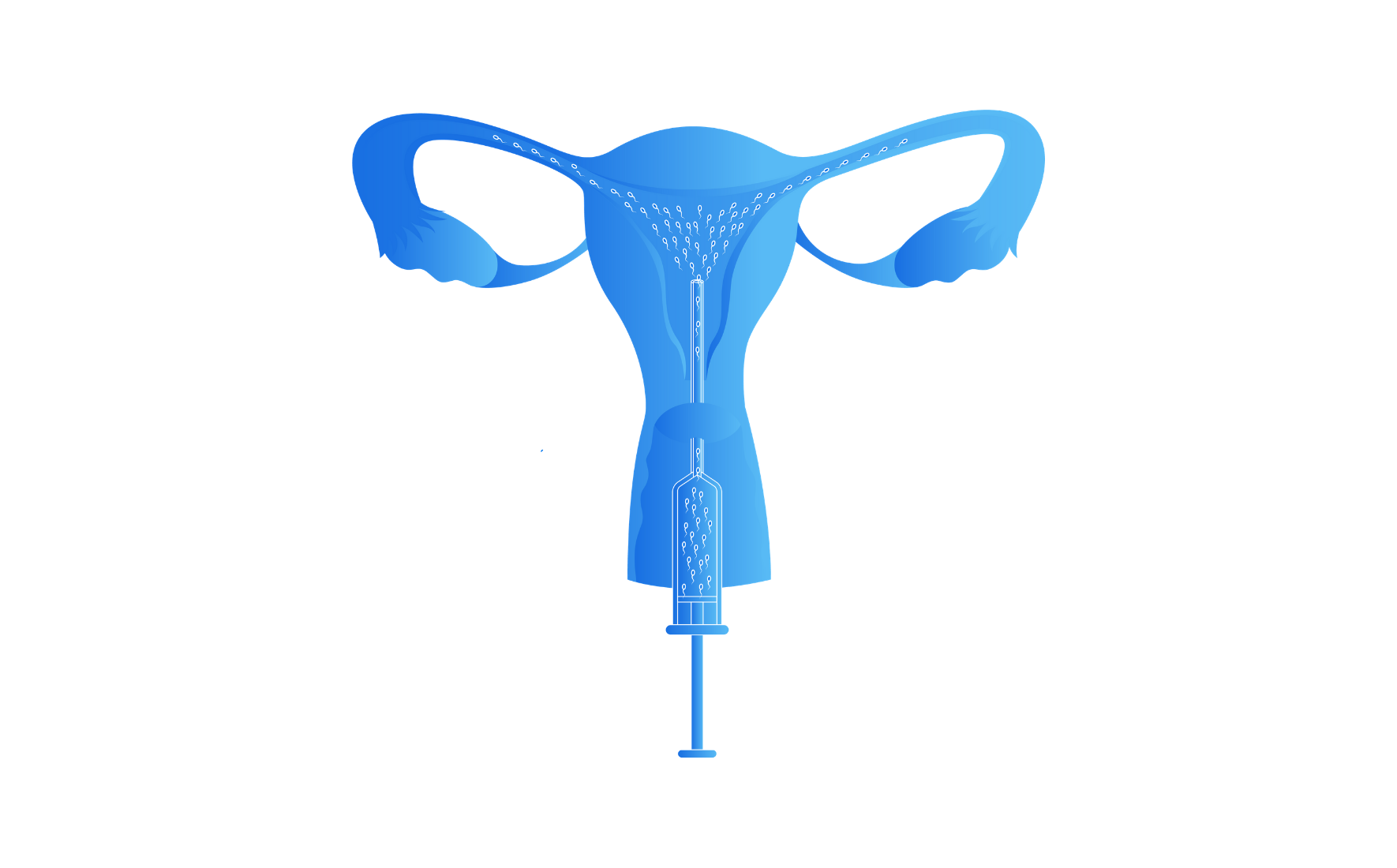
Artificial insemination is a fertility treatment in which sperm is deposited into a female’s reproductive tract using a syringe or catheter-like medical device.
Sometimes, these sperm are washed (aka cleaned, concentrated, and prepared) and the woman takes medications to increase the odds of pregnancy.
Artificial insemination was first developed by a Russian man name Ilya Ivanoff in 1899 in domesticated farm animals. The process was then later adapted for human artificial insemination with the first reports appearing around in the 1940s .
Today artificial insemination is one of the most common fertility treatments and often the first treatment one will encounter or be suggested by a medical provider. For that reason, it’s important to know the types of artificial insemination, who it can help, the process, risks, costs, and treatment alternatives.
Let’s get started!
Types of Artificial Insemination
The term artificial insemination actually refers to a few slightly different treatment methodology of placing sperm into a woman’s reproductive tract: intravaginal insemination (IVI)/intracervical insemination (ICI), and intrauterine insemination (IUI).
Because the treatment methodology for IVI and ICI are very similar and are used interchangeably to describe only one treatment – we are going to use these terms interchangeably and be discussing only two main treatments in this article: the IVI which can be done at home and the IUI which can only be done under medical supervision in an OBGYN or fertility clinic office.
What types of “infertility” can artificial insemination treat?
Pregnancy requires health sperm, eggs, uterus, fallopian tubes, and ovulation. It requires sperm travel through the cervix and uterus and into a fallopian tube to meet and fertilize an egg. The fertilized egg (now an embryo) then travels back down the tube and hopefully implants in the wall of the uterus.
However, sometimes there is no sperm (as is often the case with some LGBTQ couples and single women) or the sperm isn’t motile enough to make this trip. Other times, the woman’s cervix may not allow sperm to travel into the uterus. In these instances and other situations that prevent sperm from entering the woman’s reproductive tract or fertilizing the egg, artificial insemination may help.
A fertility specialist or other type of doctor may recommend someone pursue artificial insemination if:
- they are a lesbian couple or single woman using donor sperm.
- a heterosexual couple after six months of regular unprotected intercourse if the woman is 35 or older
- a heterosexual couple after a year of unprotected intercourse if the woman is under than age of 35
- has mild male factor infertility (problems with sperm count, motility, or shape)
- has cervical infertility
- has ovulatory infertility (often PCOS)
- has unexplained infertility
Artificial Insemination Process
The process for artificial insemination has many similarities regardless of if it’s an at-home IVI or a medically controlled fertility clinic IUI. That said, an IUI may be more involved depending on the medication protocol and monitoring requirements. That extra level of involvement with some medicated and monitored IUIs may lead to higher odds of success than an at-home artificial insemination.
At Home Artificial Insemination: The IVI
An at-home artificial insemination uses the intravaginal insemination (IVI) approach and involves depositing sperm into the vagina as close to the cervix as possible. The steps of an at-home artificial insemination include:
- Cycle and ovulation tracking: in order to properly time the ICI, a woman must track and monitor their menstrual cycle using a calendar, body temperature, urine-based ovulation predictor kits, or a combination of all the above.
- Once ovulation is detected (usually around day 14 of the cycle) a woman will lie down on their back with their hips elevated (typically using a pillow) insert an insemination syringe that has been loaded with partner or donor sperm into the vagina and deposited as close to the cervix as possible.
- It is often recommended that the woman stay lying down for 15-30 minutes. After this time they may continue their daily activity, minus hot baths that evening.
Doctors Office Artificial Insemination: The IUI
An Intrauterine Insemination IUI is a form of artificial insemination that can only be done at a doctor’s office. While it can be done in a minimally involved way in which the woman tracks their own ovulation during a natural (unmedicated) cycle and reports to the office only for the insemination, IUIs are often done with one of many possible medication protocols and coupled with bloodwork and ultrasound monitoring in order to safely track ovarian/egg development and properly time the office insemination. The general process for an IUI is as follows:
- Ovarian Stimulation: starting around days 2-4 of a woman’s cycle, one will usually begin to take a medication to help with egg development. Depending upon the medications used, they will either take those medications for around 5 or 10 days. During this time, the woman will have multiple office visits to track ovarian development and determine when the next step should take place.
- Triggering Ovulation: When doing a medicated IUI cycle, ovulation is most often “triggered” using another medication. This trigger medication usually takes place around day 13.
- Sperm Preparation & Insemination: The woman (or couple) will report to the doctor’s office for the actual insemination procedure. The sperm will be washed (unless using frozen donor sperm which has already been prepared and will just need to be thawed) and drawn into a long flexible catheter. During the procedure itself, a registered nurse, NP/PA, or physician will clean the vagina and cervix, confirm that the sperm being used is correct, and then slide the catheter (loaded with concentrated motile sperm) through the cervix and into the uterus. The sperm is then deposited into the uterine cavity and the catheter is removed.
What are the side effects and risks?
It is relatively common for a woman to experience some cramping or light bleeding following an artificial insemination.
When the artificial insemination is performed in a sterile fashion, the risk for infection is minimal. However, home inseminations open up a much greater risk of infection via contamination and an unsterile environment. Either way, it is possible that a woman experiences a pelvic infection after the procedure.
If taking medications to stimulate egg growth and ovulation, there is a significant risk of multiples such as twins or triplets .
According to the American Society for Reproductive Medicine, there is no risk of genetic or birth defects outside of those that happen during normal conception.
What Are The Success Rates?
The success rates for artificial insemination depend on a number of factors including but not limited to:
- the approach (ICI vs IUI)
- a woman’s age
- underlying fertility issues (male and female)
- use of medications
The Approach
A study published in the journal of human reproduction found that ICIs had lead to a pregnancy rate of 37.9% after 6 treatments . The same study found a 40.5 percent success rate after six treatments of IUI. This translates to a 6% per ICI try and a 7% per IUI attempt.
That said, other studies have found that there is very little difference in the overall outcome comparing the two methods when both conducted in a medical setting using the same medications .
That said, many agree that when medications are required, with specific diagnoses, or with a history of regular unprotected intercourse, an intrauterine insemination is advantageous as it offers more control and puts a substantially higher number of sperm at the uterus fallopian tube junction. ICI can still certainly be helpful – but is mainly recommended for those who can’t have sexual intercourse naturally, as an ICI places sperm in essentially the same place as intercourse.
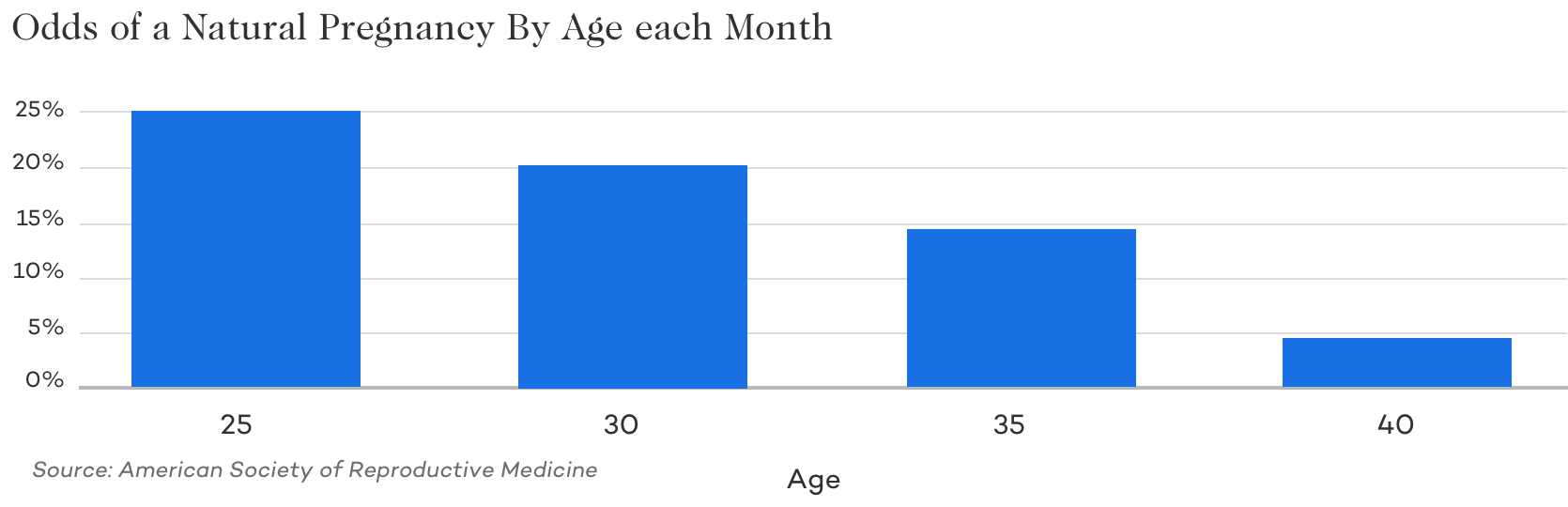
Age
It’s a well-known fact that female age contributes highly to infertility and the odds of getting pregnant each month. When you look at the odds of getting pregnant naturally each month, you’ll see a rapid decline. Because artificial insemination only assists a natural fertilization process – many of the egg and sperm quality issues effecting fertility are still significant factors when using artificial insemination.
Underlying Fertility Issues
Underlying fertility issues play a major role in the success of artificial insemination treatment.
For instance, those with PCOS who are not ovulating, the odds of a successful pregnancy by artificial insemination without medications would still be virtually zero.
Similarly, those with blocked fallopian tubes or sever male factor would have very low odds of success.
Medications
For certain individuals, like those with ovulatory issues, older women, those with diminished ovarian reserve, and others, the use of medications – both oral and injectable can result in remarkably higher odds of success. For others, the use of medications may only slightly increase the odds of a successful insemination treatment.
How much does artificial insemination cost?
The cost of an artificial insemination varies depending on many factors:
- type of treatment – at home IVI vs at office IUI
- how ovulation is being tracked – at home calendar/temperature/ovulation predictor kit vs at office ultrasound and bloodwork monitoring.
- natural vs medicated cycles
- donor sperm vs partner sperm
In general, an at-home insemination using partner sperm could cost only a handful of dollars (think $10-100) whereas an in-office IUI without monitoring or medications will typically cost at least a few hundred dollars per insemination. Add in monitoring and injectable medications and the cost per cycle will likely go up into the thousands.
There’s also the consideration of the cost per successful treatment. While an IUI is certainly the more affordable treatment on a per cycle basis, upon a closer comparison of IUI and IVF – IVF may actually be more cost-effective on a cost per live birth basis given certain diagnoses or after failing 3-4 IUIs .
Fertility Treatment Alternatives to Artificial Insemination:
While an artificial insemination either at home or in an office may be good for some people there are many reasons to consider other treatments. Any decision to pursue artificial insemination or other treatments should ideally be made in consultation with a fertility specialist after performing male and female testing.
If one’s tubes are blocked, have significant male factor infertility, diminished ovarian reserve, has tried on their own for a significant amount of time, or have other notable diagnoses it’s very possible your doctor steer you away from insemination procedures and towards in vitro fertilization (IVF). Where artificial insemination has many contraindications, IVF removes a great deal of these issues and results in the highest odds of pregnancy per treatment cycle of any treatment – for any population.
Similarly, many lesbian and trans men couples pursuing home or office inseminations choose instead to jump straight to reciprocal IVF as a way to allow both partners to be significantly involved in the child creation process.
Bottom Line
Artificial insemination is a great medical treatment. It offers same-sex couples, single parents, and heterosexual couples the chance of parenthood at a relatively low cost. At-home inseminations, while appropriate for some, aren’t highly regulated and thus can subject someone to a non-insignificant level of risk (think HIV) . Because of this and other reasons, it’s important to consult with a medical provider before making any decisions about one’s fertility treatment options.