PGT-A: Preimplantation Genetic Testing for Aneuploidy
Preimplantation Genetic Testing for Aneuploidies (PGT-A), formerly known as preimplantation genetic screening (PGS), is an embryonic procedure that checks the number of chromosomes in embryos produced via IVF.
Because the leading cause of pregnancy loss is chromosomal abnormalities in the developing fetus, PGT-A can increase the chances of a successful pregnancy by identifying chromosomally normal embryos for transfer. PGT-A can also be used by couples who wish to select the sex of their intended child, also known as gender selection.
This article will explain the details of PGT-A testing, who are good candidates, the associated costs, and more!
Fast Facts about PGT-A Testing
- PGT-A stands for Preimplantation Genetic Testing for Aneuploidies and is an embryonic procedure done on IVF embryos that looks at the chromosomes inside the cells of an embryo.
- Embryos are classified with one of three potential results from PGT-A testing; euploid (normal), mosaic (partially normal, partially abnormal), and aneuploid (abnormal).
- As women get older, their chances of getting pregnant decrease. This is largely driven by the increased percentage of abnormal eggs and the resulting aneuploid embryos they produce.
- By identifying abnormal embryos, PGT-A can reduce the chance of miscarriage compare by selectively transferring embryos that have the correct number of chromosomes.
- By identifying the best embryo(s) for transfer (euploid or normal), PGT-A testing can increase the live birth rate per IVF embryo transfer. However, during PGT-A testing, some embryos may be identified as abnormal, which eliminates them from consideration for transfer. As such, it is unclear whether or not PGT-A increases the chance of a live birth per IVF egg retrieval.
- PGT-A can also be used for gender selection.
- Other types of genetic testing can be performed if the intended parent(s) is at high risk of having a child with a specific genetic disease, or one or both parents has a known chromosomal abnormality.
What is PGT-A Testing?
PGT-A is an embryonic procedure done during the IVF Process that checks the number of chromosomes for each embryo prior to the embryo transfer portion of IVF treatment.
A normal embryo contains 23 pairs of chromosomes, for a total of 46 chromosomes (euploid). 23 chromosomes come from the sperm and 23 from the egg.
Twenty-two of these pairs (autosomes) look the same for both males and females. However, the 23rd pair (sex chromosomes) differ between males and females. This is because females have two X chromosomes in their cells, and males have an X and a Y chromosome in their cells.
The example below shows a normal, or euploid chromosomal count on the left and an abnormal chromosomal count on the right given chromosome 10 has 3 copies as opposed to the two it should have.
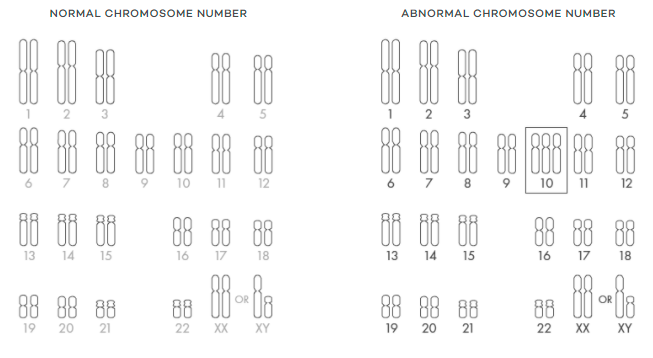
Embryos with more or less than 46 chromosomes (aneuploid) can cause IVF transfers to fail, pregnancy loss, or significant health problems for your child.
PGT-A testing can increase the chances of a successful IVF transfer by ensuring embryos have the correct number of chromosomes. Because you can see the sex chromosomes, PGT-A testing can also be used to select embryos of a certain sex, also known as gender selection.
How is PGT-A Performed?
Step 1: Tissue Biopsy
The first step of PGT-A testing is performed after the ovarian stimulation, egg retrieval, fertilization, and embryo development stages of the IVF process. After embryos reach the blastocyst stage of development (approximately 5-7 days after fertilization), a tissue biopsy is performed, and a small cell sample is taken from each embryo and frozen.
Step 2: Sample Shipping and Embryo Freezing
Next, the tissue samples are shipped to the genetics lab where testing will occur. Meanwhile, the embryos are frozen via vitrification, and they are stored until it is time for the frozen embryo transfer.
Step 3: PGT-A Chromosomal Analysis
After the tissue sample(s) reach the genetics lab, then the PGT-A chromosomal analysis is completed. During the analysis, embryos are screened for chromosomal abnormalities and the sex chromosomes are checked.
Step 4: The Genetics Report
After the analysis is completed, the genetics lab will send a genetics report detailing the status of each embryo, including the sex and number of chromosomes, back to the fertility center. The fertility specialist will review the genetics report and share the results with the patient.
Step 5: Embryo Selection and Frozen Transfer
Based on the results outlined in the genetics report along with the input from the provider and patient, the embryologist will select the healthy embryo(s) of the desired sex for transfer. The selected embryo(s) will then be thawed and prepped when it is time for the embryo transfer.
If there are remaining embryos, they will stay frozen and stored for use at a later time.
PGT-A Testing Results
PGT-A testing can produce three different types of results for each embryo:
- Euploid (Normal) – All cells sampled from the embryo have 46 chromosomes
- Mosaic (Mixed) – some cells that were tested in the embryo are normal, some are abnormal.
- Aneuploid (abnormal) – all cells obtained from the biopsy had an abnormal number of chromosomes.
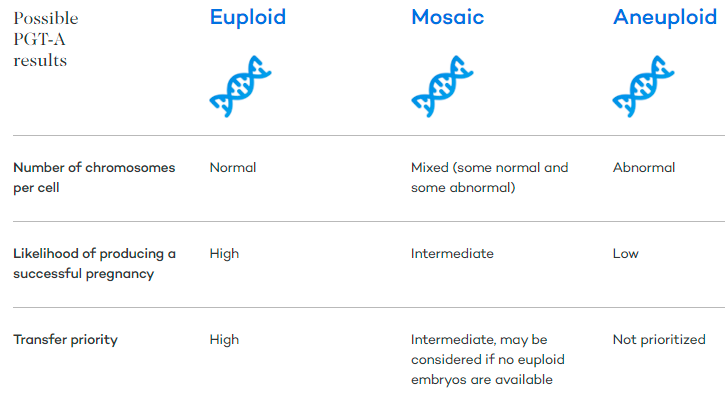
Euploid embryos are the most desired as they produce the greatest chance for a successful pregnancy. Mosaic embryos can have different proportions of abnormal cells. A low-level mosaic embryo has mostly normal cells and a lower percentage of abnormal cells. After euploid embryos have been transferred, or if all resulting embryos come back as mosaic or aneuploid, then mosaic embryos may be considered for transfer.
Research shows that although mosaic embryos result in inferior clinical outcomes compared to euploid embryos, they can result in healthy pregnancies and babies .
Candidates for PGT-A Testing
PGT-A testing can be completed by anyone undergoing an IVF procedure without known genetic diseases. That said, PGT-A is primarily recommended for females over 35 (especially if they have a history of failed IVF implantation or pregnancy loss) and those wishing to choose the sex of their child.
If a patient is considered high risk for passing along a certain genetic disease to their offspring, or if they have a known chromosomal rearrangement, then a different type of genetic testing should be completed (more on that to come).
Those with a Female Partner 35 or Older
As women get older, the percentage of abnormal eggs they produce increases. Eggs with chromosomal abnormalities result in embryos with chromosomal abnormalities. Embryos with chromosomal abnormalities generally do not result in a live birth and thus an increase in maternal age usually results in a lower chance of getting pregnant.
As displayed in the figure below, the percentage of genetically abnormal embryos increases significantly after women reach the age of 35. Therefore, women over the age of 35 may wish to consider PGT-A testing, especially if they have a history of failed implantation or pregnancy loss.
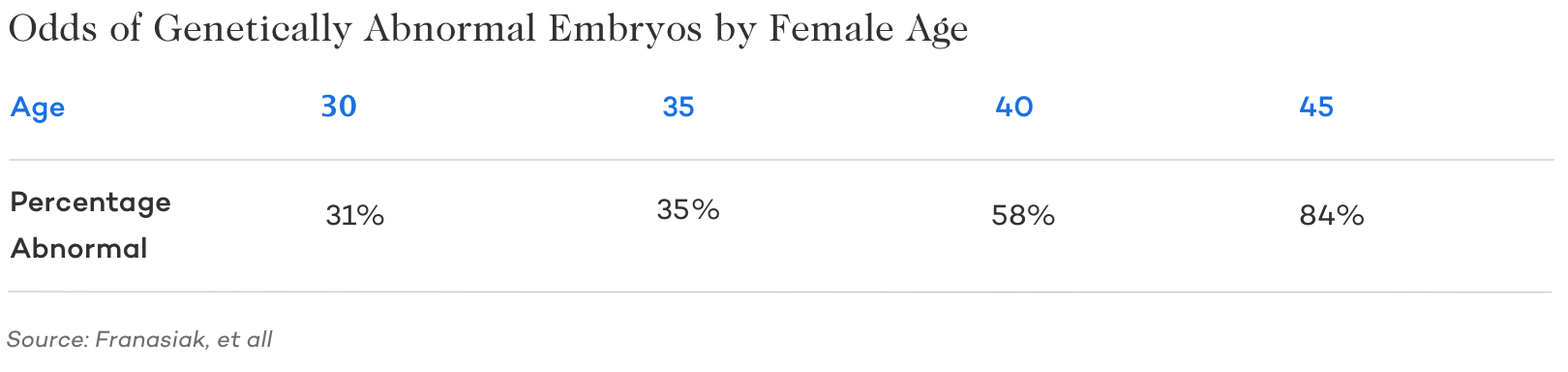
As you would expect, since the percentage of abnormal (aneuploid) embryos increases with age, the percentage of normal euploid and mixed mosaic embryos produced also decreases as these are inversely proportional.
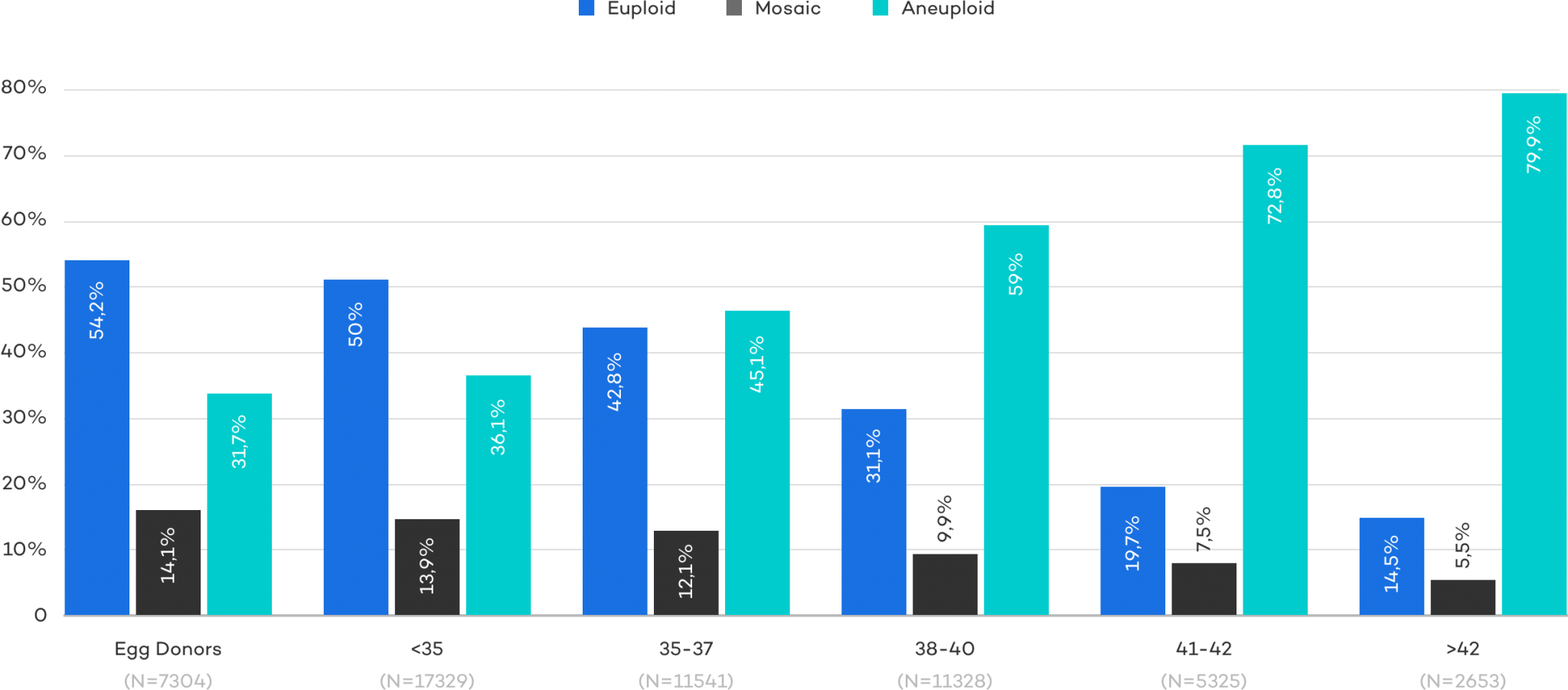
As previously mentioned, euploid embryos are the most desired and produce the highest rate of success per embryo transfer. However, mosaic embryos can also produce viable offspring. Since the proportion of euploid and mosaic embryos decreases over time, it makes sense that live birth rates also decrease as women age, but more on that below.
Fortunately, PGT-A testing can help increase the chances of successful implantation by ensuring that only high-quality embryos with the correct number of chromosomes are transferred.
Gender/Sex Selection
Other candidates for PGT-A testing are those who wish to select the sex of their intended child. As mentioned above, the resulting genetics report from PGT-A testing will include information about the sex chromosomes of each embryo. If an embryo has XX sex chromosomes it is a female, and if it has XY chromosomes it is a male embryo.
Other Candidates
Other candidates for PGT-A testing are mainly those at a higher risk of producing irregular embryos, such as:
- Women suffering from recurrent pregnancy loss
- Women who have experienced repeated implantation failure
- Couples where the male partner has severe male factor infertility
PGT-A Success Rate and Miscarriage Statistics
As mentioned above, PGT-A has a powerful ability to see inside an embryo and determine if it has any major chromosomal abnormalities. Because pregnancy loss is often caused by these same genetic abnormalities, PGT-A certainly seems like it should have the ability to reduce pregnancy loss and overall success rates.
While incredibly promising, most data indicates it’s only beneficial for some patient populations and even that isn’t always conclusive. Because of this, it’s important to discuss the pros and cons of PGT-A with your reproductive endocrinologist.
PGT-A to Reduce Miscarriage Rates
Research has shown that abnormal embryos can significantly increase the chances of miscarriage.
Because PGT-A allows you to selectively transfer embryos with a normal genetic profile, the odds of pregnancy loss are generally much lower.
Check out the figure below to see an illustration of Cooper Genomics data on how PGT-A testing decreased the rate of miscarriage across age groups – particularly notable is the data as one gets closer to and beyond 40.
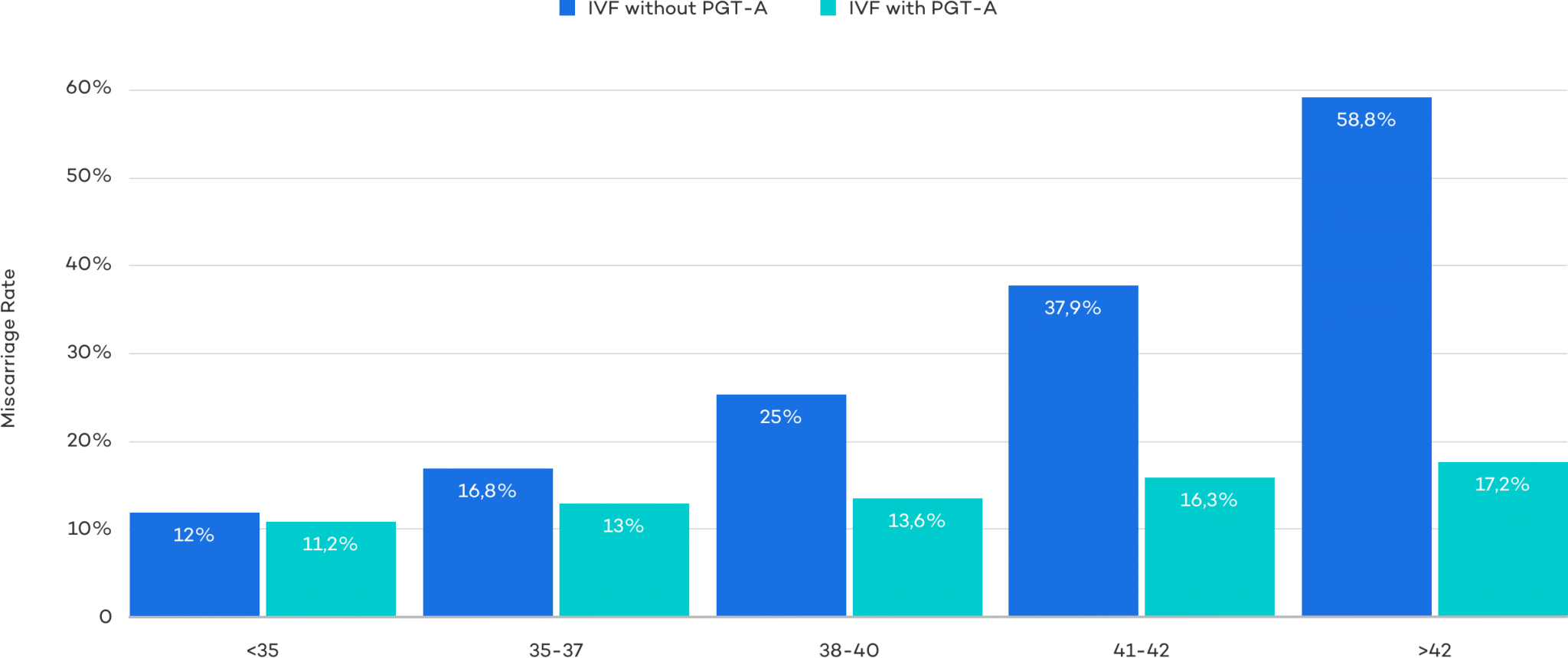
That said, the results aren’t always so clear. While a 2018 committee report confirms the above and shows data that PGT-A testing reduces miscarriages, a large 2019 study found no difference.
Given the conflicting data, it’s hard to draw definitive conclusions. That said, most experts lean on the side of caution and appreciate PGT-A as a valuable tool.
Miscarriage can cause both physical and emotional stress for the intended parent(s) and waste valuable time in the pursuit of bringing a child into the world. By decreasing the chances of miscarriage, PGT-A may help protect from the stresses of miscarriage, the amount of time it takes to get pregnant, and as we will see below, increase the success rates of IVF embryos transfers.
PGT-A and Success Rates
A 2015 meta analysis that reviewed several small studies found a benefit in the overall success rate when using PGT-A. Two other studiesy conducted in 2016 and 2017 found an increase in success rates with PGT-A, but only in females older than 37.
From 2014 to 2017, Cooper Genomics collected data of blastocyst biopsies and transfers. As you can see from the figure below, PGT-A testing and its ability to identify the best embryos resulted in increased live birth rates for women across all age groups. The disparity between live birth rates for IVF without PGT-A and IVF with PGT-A grows noticeably as the female ages.
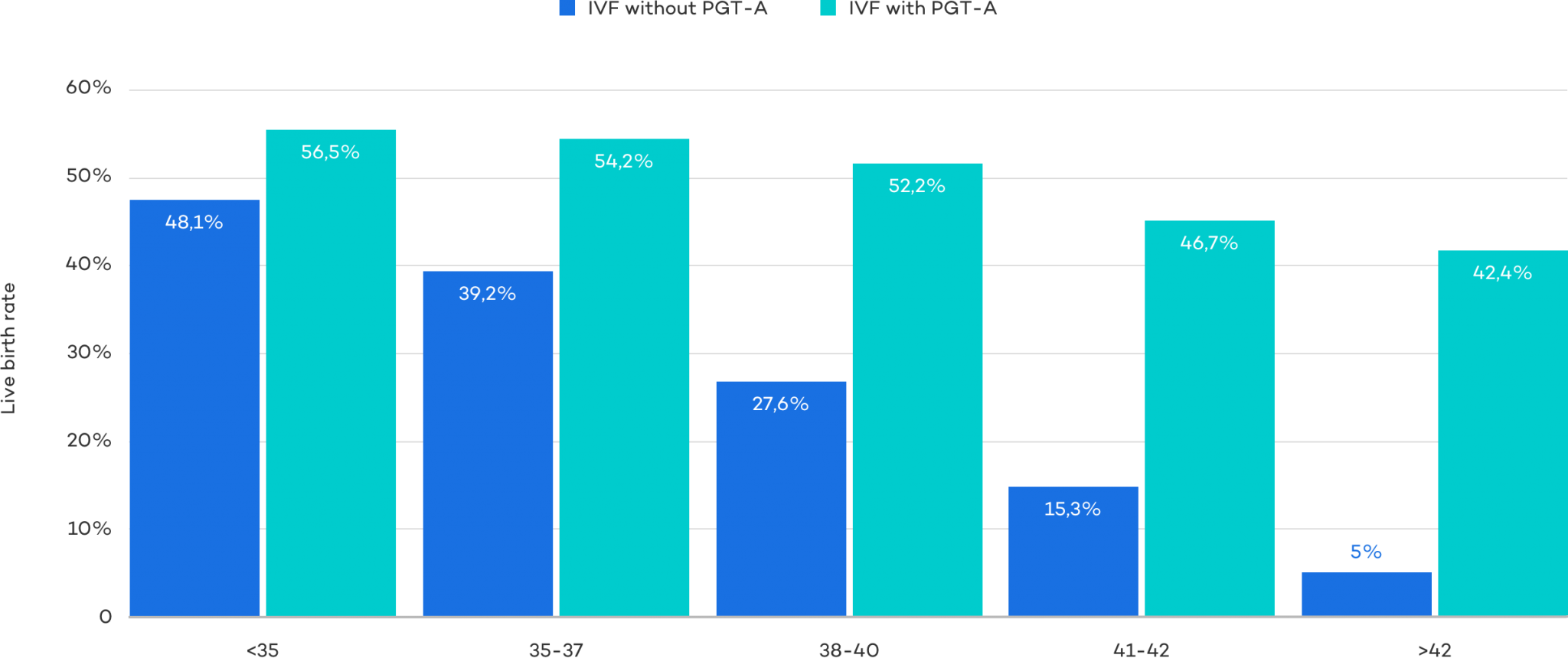
In 2019, a large study supported a similar notion and found that while there was no difference when using PGT-A testing across ages 25-35, success rates increased from 37.2% to 50.8% in the 35-40-year-old group.
More Issues with PGT-A Success Rate Data
Although the data above seems significant, there are other variables that must be considered. Since PGT-A testing identifies the best embryo(s) for transfer, it makes sense that the live birth rate per transfer would be higher. However, this doesn’t mean the live birth rate per IVF retrievals is higher. In fact, PGT-A actually has the possibility of decreasing the chance of pregnancy per IVF cycle.
A study was conducted between 2012 and 2016 to measure the effects of PGT-A testing on IVF with ICSI success rates for women between the ages of 36 and 40. Of the 396 women that were enrolled in the study, 205 had embryo testing, 191 did not.
After one year, 50 of the 205 (24%) of the women in the PGT-A testing group had a live birth, compared to 45 of the 191 (24%) in the group without PGT-A testing. While there was no statistical difference in the live birth rates between the two groups the number of embryos transferred was significantly lower for the embryo testing group as was the miscarriage rate.
This study highlights the fact that PGT-A testing can result in viable embryos being mistakenly discarded. There are two ways embryos can be mistakenly discarded.
Embryos may be able to correct themselves
While it isn’t yet conclusive, some evidence suggests that mosaic embryos can self-correct and over time, develop into a euploid embryo. Mosaic chromosome abnormalities are common in early human embryos and research has shown mosaic embryos can result in healthy pregnancies.
In a study published by the American Study for Reproductive Medicine (ASRM), 32 women elected to have at least one mosaic embryo transferred. 11 women (34%) had successful pregnancies which resulted in healthy babies.
A non-representative biopsy sample
Another issue that could cause embryos to be mistakenly discarded is due to a non-representative sample being taken from the embryo. Most biopsies only take 5 or so cells compared to 300 or so cells that exist in the embryo in the blastocyst stage. Interestingly one study found that you’d need at least 27 cells from a biopsy to be confident that the biopsy matched the rest of the embryo. The problem is that taking this many cells could fatally damage the embryo.
The below graphic illustrates this problem.
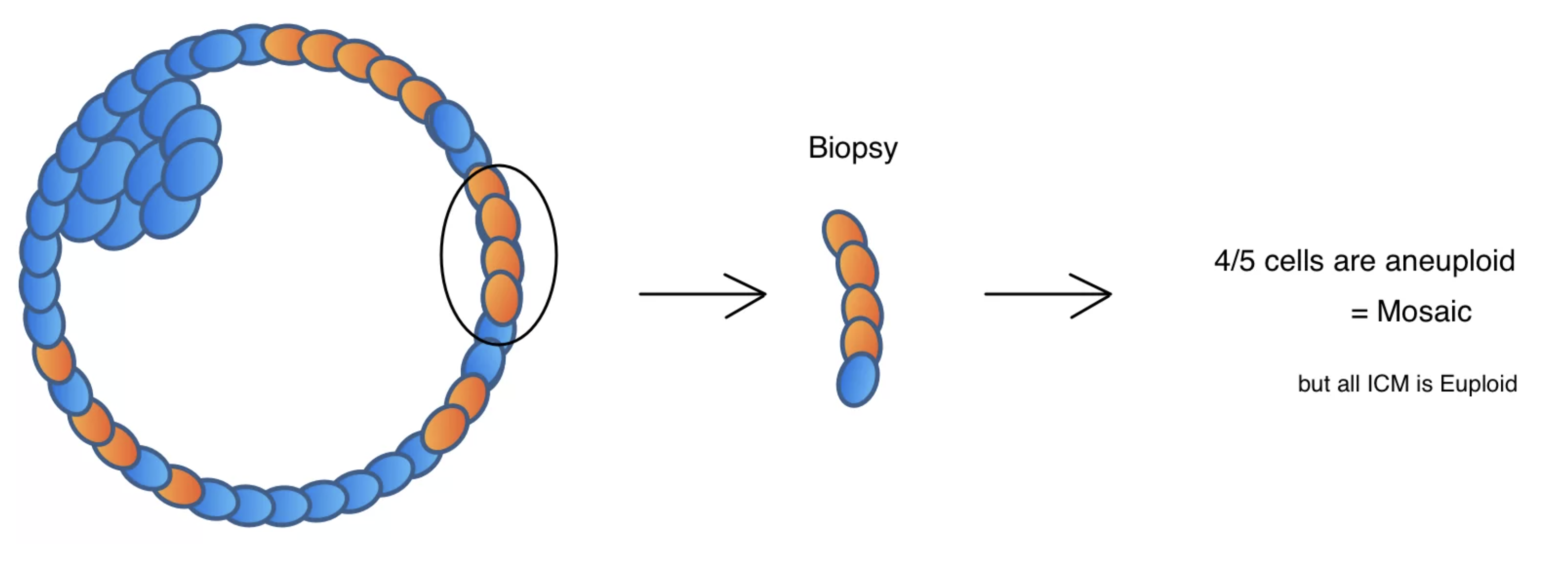
In the example above, the Inner Cell Mass (the part of the embryo that becomes the baby) is normal, and the trophectoderm (the outer ring where the biopsy is taken from ) is mosaic. The example becomes worse if only abnormal cells are removed from what is truly a mosaic embryo with a 100% normal ICM during the biopsy; the PGT-A testing would misclassify the embryo as abnormal and would thus be discarded.
+ Learn more about the risks of embryonic genetic testing
How Much Does PGT-A Cost?
PGT-A testing is most commonly performed in conjunction with an IVF procedure which starts at a cost of $4,500 at CNY Fertility. Including monitoring, medications, and genetic testing we estimate the total cost to be around $12,000 at CNY which is comparable to the national average of $27,500.
The price of PGT-A testing itself is variable depending on the number of embryos being tested and is split between CNY Fertility embryo biopsy fees and the genetic lab testing fees Total prices (including CNY embryo biopsy fees and genetics lab fees) are generally in the $2,000-3,000 range.
We encourage you to explore the cost of IVF with PGT-A along with our financing options using the treatment calculator below.
Automatically Included
- {{ tick.item }}
Sample Payment Calculator: Self Pay Pricing
- {{getTreatmentName()}} {{ treatment_price_discount|toCurrency }}
National Average {{ this.treatment_price_others|toCurrency}} - {{ treatment.data.price.monitor.remote.label }} Remote Cycle Management {{ total_monitor.cny | toCurrency }}{{ treatment.data.price.monitor.in_house.label }} In House Monitoring {{ total_monitor.cny | toCurrency }}{{ treatment.data.price.monitor.remote.note_calc | stripHTML }} {{ treatment.data.price.monitor.in_house.note_calc | stripHTML }} Third-party fixed fee (SAMA) Third Party {{ total_monitor.others | toCurrency }}{{ treatment.data.price.reciprocal_ivf.note_calc || "Reciprocal IVF requires both partners to be monitored" }} {{ treatment.data.price.frozen_transfer.note_calc_monitor || "" }}
- {{ treatment.data.price.frozen_transfer.label }} Frozen Transfer {{treatment.data.price.frozen_transfer.cny|toCurrency}}
- {{ treatment.data.price.cryo_preserve.label }} Cryopreservation + 1yr Storage {{treatment.data.price.cryo_preserve.cny|toCurrency}}{{treatment.data.price.cryo_preserve.note_calc | stripHTML}} Third Party {{treatment.data.price.cryo_preserve.others|toCurrency}}
- {{ treatment.data.price.genetic_testing.label }} Genetic Testing {{treatment.data.price.genetic_testing.cny|toCurrency}}{{treatment.data.price.genetic_testing.note_calc | stripHTML}} Third Party {{treatment.data.price.genetic_testing.third_party|toCurrency}}
- {{ treatment.data.price.medication.label }} Medication Estimate {{total_medication.cny|toCurrency}}{{total_medication.note_calc | stripHTML}} Third Party {{total_medication.third_party|toCurrency}}
- {{ treatment.data.price.medication.label }} Medication Estimate {{total_medication.cny|toCurrency}}{{total_medication.note_calc | stripHTML}} Third Party {{total_medication.third_party|toCurrency}}
- {{ treatment.data.price.zymot.label }} ZyMōt Sperm Processing ${{treatment.data.price.zymot.cny}}{{ treatment.data.price.zymot.note_calc | stripHTML}} Third Party ${{treatment.data.price.zymot.third_party}}
- {{ treatment.data.price.pregmune.label }} Pregmune Reproductive Immunology Testing {{treatment.data.price.pregmune.cny|toCurrency}}{{ treatment.data.price.pregmune.note_calc | stripHTML}} Third Party {{treatment.data.price.pregmune.third_party|toCurrency}}
- {{ treatment.data.price.donor_eggs.label }} Donor eggs {{total_donor_eggs.cny|toCurrency}}{{treatment.data.price.donor_eggs.note_calc | stripHTML}} Third Party {{total_donor_eggs.others|toCurrency}}
- {{ treatment.data.price.donor_sperm.label }} Donor sperm {{treatment.data.price.donor_sperm.cny|toCurrency}}{{treatment.data.price.donor_sperm.note_calc | stripHTML}} Third Party {{treatment.data.price.donor_sperm.others|toCurrency}}
- {{ treatment.data.price.donor_eggs.label }} Donor Package {{total_donor_package.cny|toCurrency}}{{treatment.data.price.donor_package.note_calc | stripHTML}} Third Party {{total_donor_package.others|toCurrency}}
- {{ treatment.data.price.gestational_surrogacy.label }} Gestational Surrogacy {{treatment.data.price.gestational_surrogacy.cny|toCurrency}}{{treatment.data.price.gestational_surrogacy.note_calc | stripHTML}} Third Party {{treatment.data.price.gestational_surrogacy.others|toCurrency}}
- {{treatment.data.price.split_cycle.label ? treatment.data.price.split_cycle.label : "Split Cycle Discount" }} {{discount_split_cycle|toCurrency}}
- 5% Military & Veteran Discount {{discount|toCurrency}}
- Installments Fee {{finance.fee|toCurrency}}
- Total to CNY {{total.total | toCurrency}}
Estimated 3rd Party Costs {{total.third_party| toCurrency}}
Grand Total {{(total.total + total.third_party)| toCurrency}}
National Average: {{total.national|toCurrency}} - Down Payment to CNY{{finance.payment_down_amount|toCurrency(2)}}
- Monthly Payment to CNY{{finance.monthly_payment|toCurrency(2)}}
{{ treatments[treatment_selected]['data']['footnote'] }}
The above calculation is for simulation purposes only. It is reflective of self-pay pricing, includes highly variable estimates paid to CNY and third parties, and national averages obtained through internal research, FertilityIQ, ASRM, and Resolve. Billing through insurance will likely result in substantially different fees. CNY Fertility does not warrant or guarantee any price for services conducted or rendered by a third party and recommends everyone obtain written estimates from any medical facility involved in your treatment as well as verification of coverage from your insurance company prior to beginning treatment.
1 USD = {{currency.rates[currentCurrency]}} {{currentCurrency}}
Last Update {{currency.last_update}}
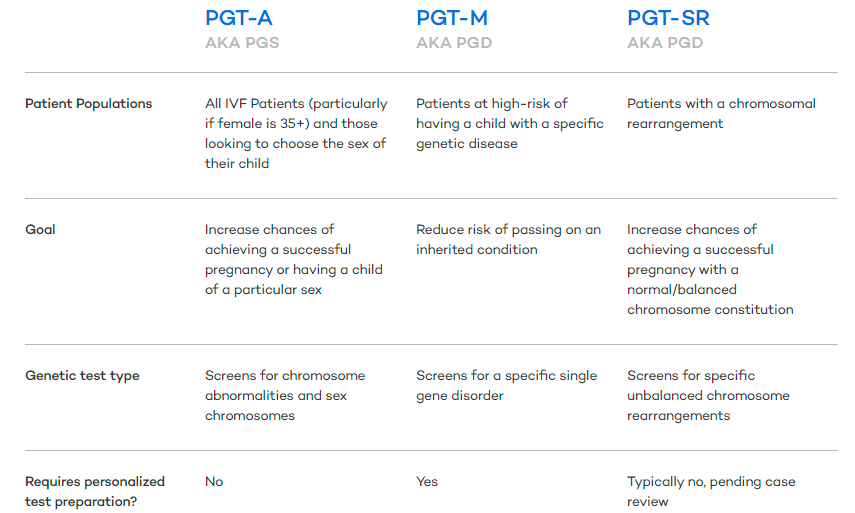
Other Types of Genetic Testing
If the intended parent(s) is at high risk of having a child with a specific genetic disease, or one or both parents has a known chromosomal abnormality then alternate forms of genetic testing are recommended. While PGT-A testing does not require any pre-testing or individualized test preparation, the other types usually do.
Check out the chart below for information on all three types of genetic testing PGT-A, PGT-M, and PGT-SR.
The Bottom Line about PGT-A Testing
PGT-A testing can help increase the chances of success per embryo transfer by identifying abnormal embryos and ensuring the embryo(s) being transferred have the correct number of chromosomes. PGT-A testing does not however guarantee greater success per IVF cycle. There are associated risks and other considerations that should be discussed with a fertility specialist.
PGT-A can also be used for gender selection which is utilized by many couples who wish to balance their families or for a number of other reasons.
If you are considering IVF, genetic testing, or any other fertility treatments, schedule a consultation with one of our providers and discuss your options with the most affordable fertility clinic in the nation. Don’t worry if you aren’t located near one of our clinics, as over 1/2 of our patients travel for treatment from out of state and out of the country.
We look forward to assisting you on your fertility journey!