IUI Success Rates: Factors and Solutions

If you’re considering Intrauterine insemination (IUI) as a fertility treatment, you’re probably curious about IUI success rates.
IUI, sometimes called artificial insemination, works by bypassing the vagina and cervix to place concentrated sperm directly into the uterus, closer to the egg. This “head start” can increase the chances of fertilization. But just how likely is it to lead to pregnancy?
As with most fertility treatments, success rates depend on a number of factors, from age and diagnosis to sperm quality and the use of medications.
In this article, we’ll explore everything you need to know about IUI success rates, share practical ways to improve them, and highlight inspiring success stories to keep hope alive. But first, let’s start with a quick overview before diving deeper.
Fast Facts About IUI Success Rates
Overall Success Rates: Across all patient types, IUI cycles typically result in live birth rates of 5–15% per cycle. Reported outcomes vary widely, with some studies showing as low as 8% success (even with fertility drugs) , while others report rates above 20%. Factors like age, diagnosis, and whether fertility medications are used all play a major role.
Cumulative Success: Success builds with repetition. Most research shows that 90–95% of successful IUIs occur within the first 3–4 cycles. Beyond that, chances of success drop significantly.
Not for Everyone: Because IUI still relies on natural conception, where sperm must swim through the fallopian tubes, fertilize an egg, and implant in the uterus, it isn’t effective for specific diagnoses. In cases like blocked tubes or severe male factor infertility, success rates are close to zero.
Defining Success: IUI “success” can mean different things, from a positive pregnancy test to a live birth, and may also include consideration of multiple pregnancy risk.
Individualized Outcomes: Since success rates vary significantly depending on age, the type of fertility drugs used, and the underlying diagnosis, it’s essential to discuss your specific situation during your consultation with a fertility specialist.
IUI Success Rates by Diagnosis and Patient Demographics
By Age:
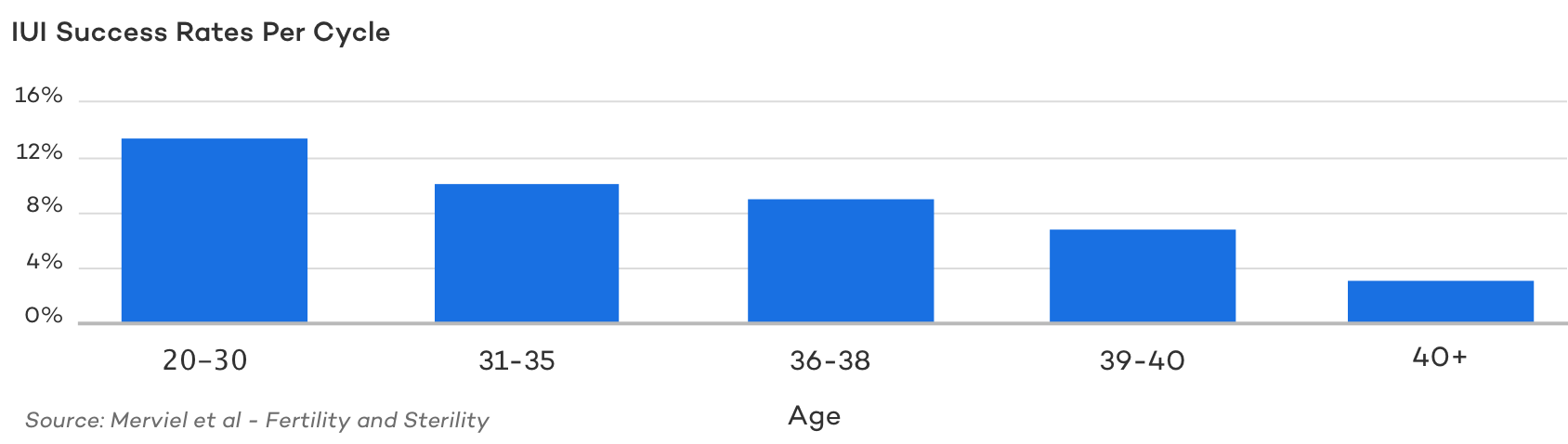
Outside of certain specific fertility diagnoses, age is the single most important factor in determining the likelihood of IUI success.
As women get older, egg quality declines, conception rates drop, and more IUI cycles are often required to achieve pregnancy. Because of this, most fertility specialists do not recommend IUI for women over 40.
For women under 35, ideal candidates can expect about a 15–20% chance of success per cycle. Between the ages of 35 and 40, that chance drops to around 10% per cycle, and for women over 40, success rates fall to 5% or less per cycle. , other studies predict even lower odds.
For Patients with Ovulatory Issues or PCOS
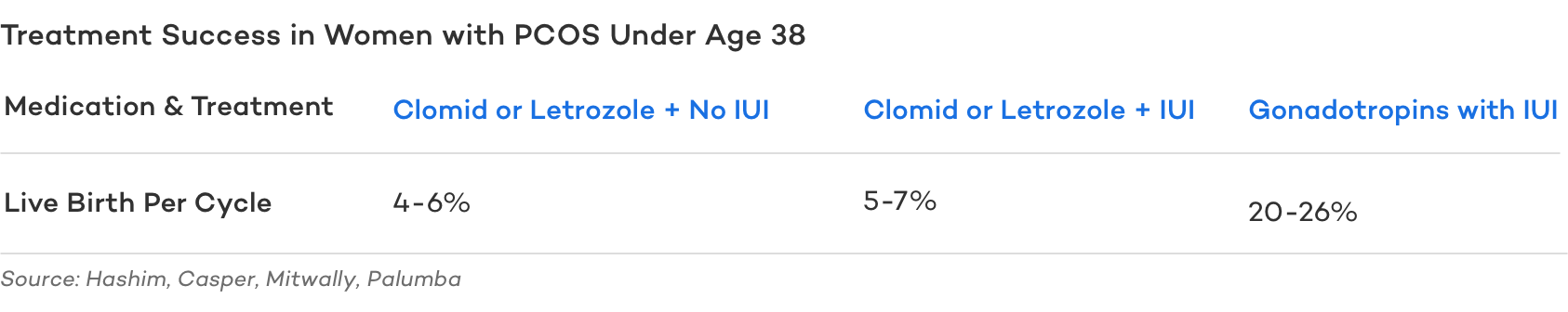
Women who don’t ovulate (anovulation), have absent or irregular menstrual cycles, or have been diagnosed with PCOS, the most common ovulatory disorder affecting one in ten women, often require medications to conceive.
While Letrozole is the preferred medication for PCOS based on a double-blind, randomized study (especially for women with a BMI over 30 kg/m2), some women have better success with Clomid. Others may be resistant to both Letrozole and Clomid and require gonadotropins to ovulate.
IUI can only be effective for patients with PCOS if ovulation actually occurs. Combining IUI with a medicated cycle using Clomid or Letrozole offers a modest increase in conception rates, particularly when mild male factor infertility is present and sperm motility is less than ideal.
For women with PCOS who require gonadotropins, IUI has been shown to significantly improve the chances of conception.
For Patients with Male Factor Infertility
Men with mild male factor infertility and their partners may benefit from IUI, but those with severe sperm issues generally do not.
This is because IUI functions as a facilitator of natural conception. While it gives sperm a “head start” by placing them directly into the uterus, fertilization still depends on the sperm’s ability to travel through the fallopian tubes and reach the egg.
If the male partner has a very low sperm count, the likelihood of sperm reaching the egg on their own is minimal. In such cases, IVF with intracytoplasmic sperm injection (ICSI) is usually recommended. If no sperm are present in the ejaculate at all, surgical retrieval from the reproductive tract may be an option.
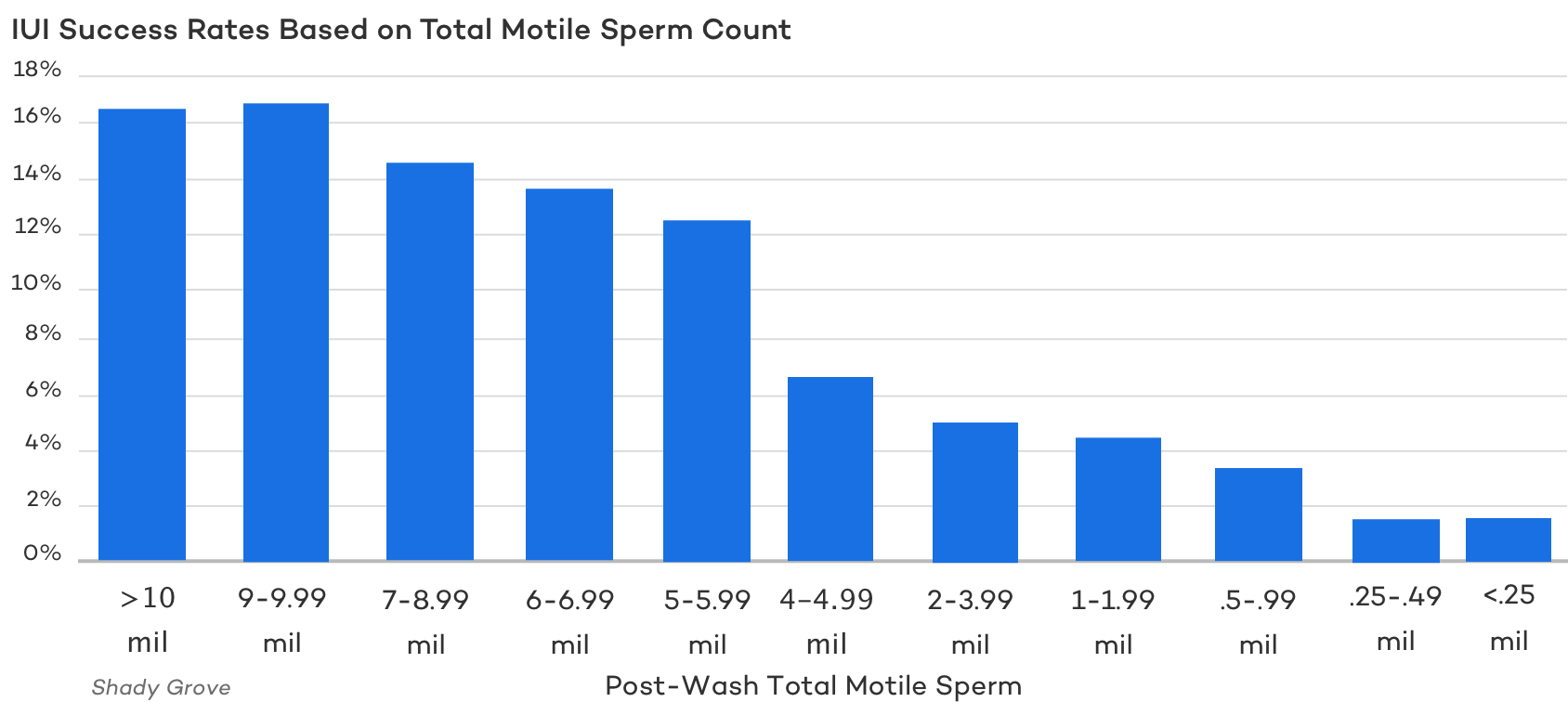
So, what defines mild versus severe? Each fertility clinic sets its own parameters. At CNY Fertility, IUI is generally not recommended for patients with fewer than 7 million total motile sperm.
A 2015 retrospective study of more than 47,500 IUI cycles evaluated fresh post-wash total motile sperm counts (typically up to 30% lower than pre-wash counts) and their relationship with pregnancy rates. The study found that couples with a post-wash total motile sperm count of at least 9 million had a per-cycle pregnancy rate of 16.9%. Success rates plateaued above this threshold but declined steadily for patients with counts below 9 million.
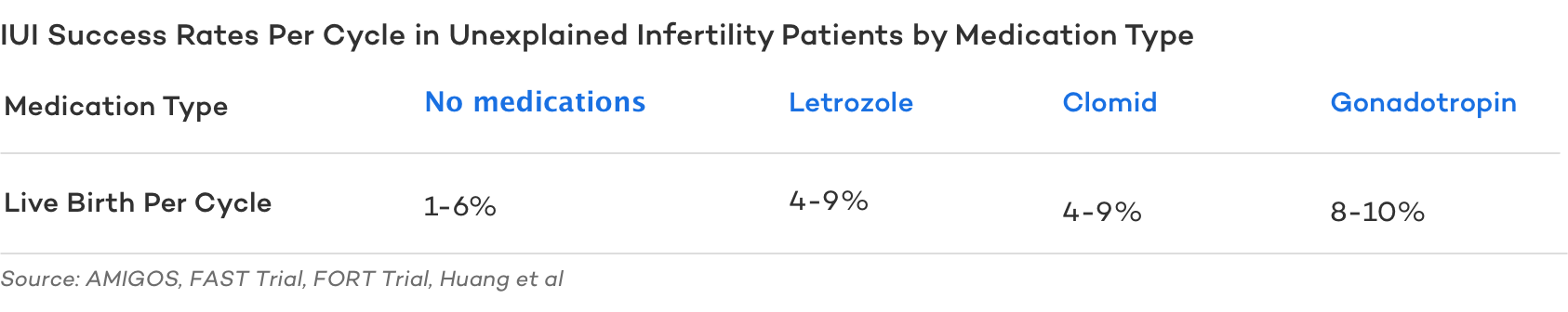
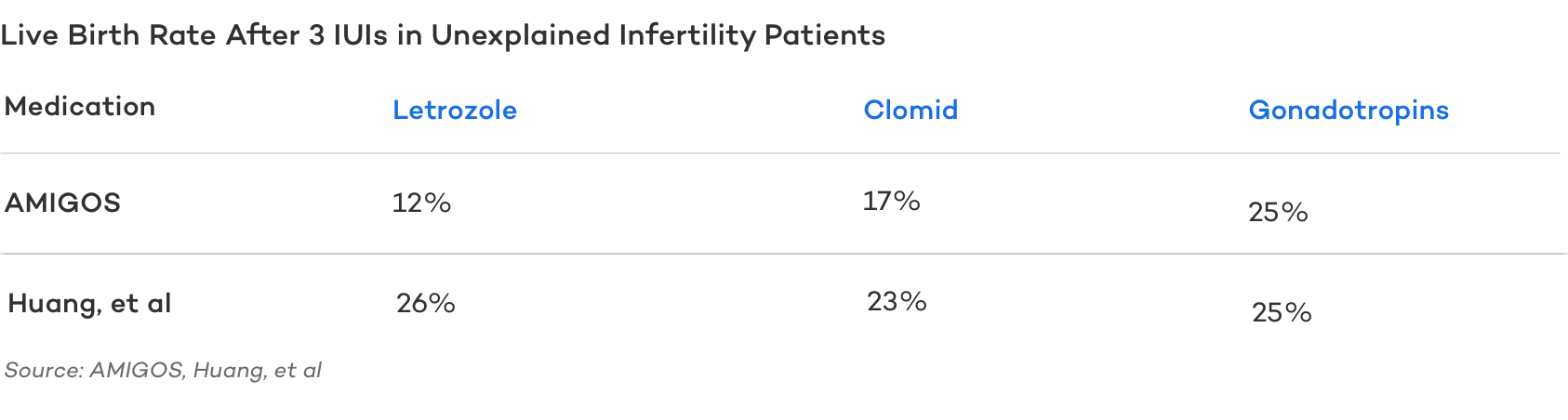
For Patients with Unexplained Infertility
A diagnosis of “unexplained infertility” usually means you have a good egg count, open fallopian tubes, a healthy uterus, sperm count within normal parameters, and no other explanation for difficulties conceiving.
This group includes up to 25% of women experiencing fertility challenges. Women in this category can expect IUI success rates of 7-10% per cycle. After 3 medicated IUI cycles with Letrozole or Clomid, success rates can range from 15-25%.
Single Open Fallopian Tube
Fortunately, it only takes one open fallopian tube to achieve pregnancy. If a woman has one blocked tube and one open tube, conception is still possible, although success rates vary depending on the location of the blockage.
Women with a blockage in the distal portion of the tube (near the ovary) generally have poorer outcomes compared to those with a proximal blockage (closer to the uterus). This difference is partly because hysterosalpingograms (HSGs) can misdiagnose a proximal blockage in up to 30% of cases, even when the tube is actually open.
- Women under the age of 38 undergoing IUI with a proximal tubal blockage and one open tube had a cumulative conception rate of about 38.1% after three cycles.
- Women with a distal blockage had only around an 11.7% chance of conceiving.
Single and Lesbian Women
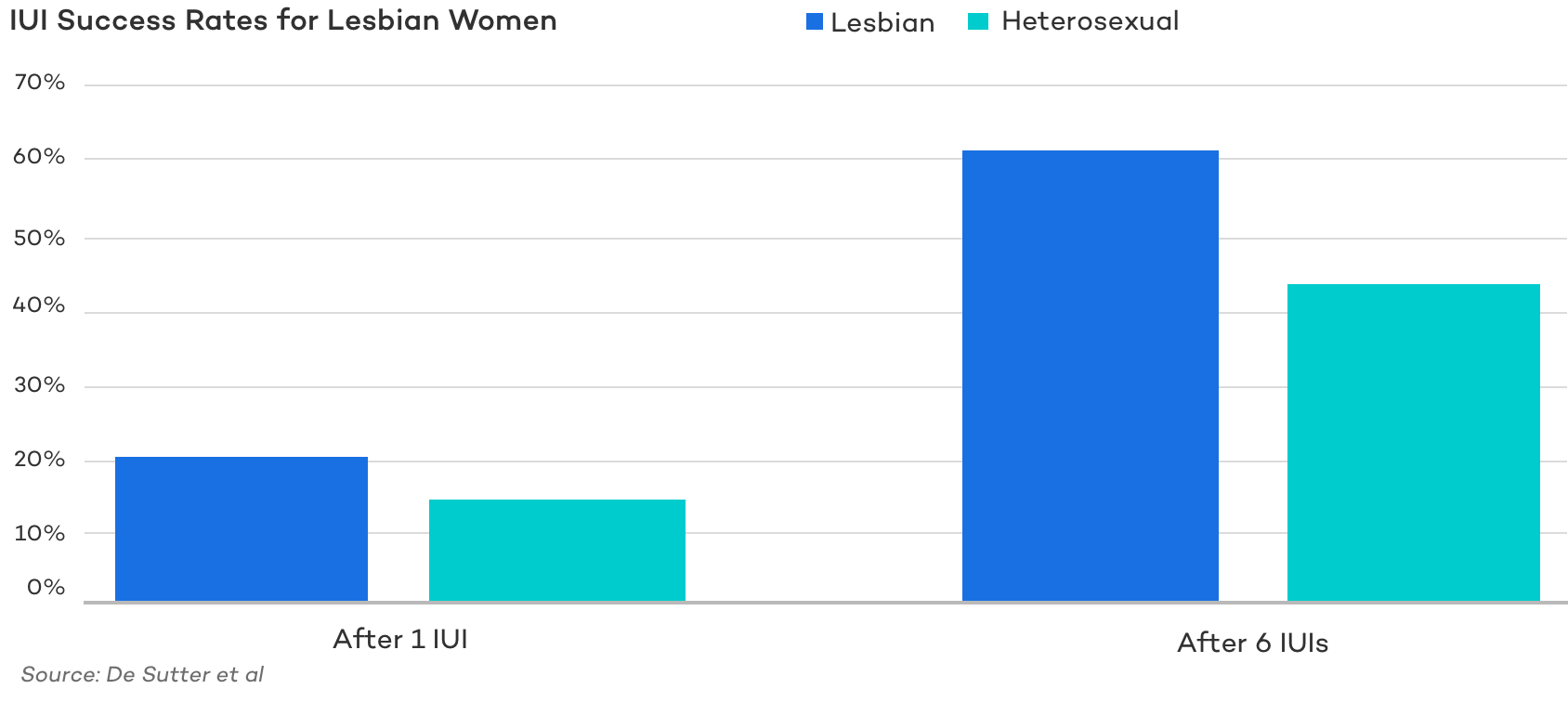
Single women and lesbian couples often have excellent outcomes with IUI, even during unmedicated cycles, because there is usually no underlying fertility issue, and the sperm used is typically high quality from screened donors.
A 2014 study showed that lesbian women had significantly higher pregnancy rates from IUI compared to heterosexual women. After one cycle, lesbian women had a 20.5% pregnancy rate versus 14.8% in heterosexual women. After three cycles, the cumulative rates rose to 61.6% and 44.0%, respectively.
An earlier study examined lesbian women (ages 26–44) and single women (ages 29–47) using frozen donor sperm. The researchers found a clinical pregnancy rate of 57% in lesbian women compared to 36% in single women.
After six IUI cycles, the cumulative pregnancy rates increased to 70% and 47%, respectively.
The study authors concluded that lower success rates in single women were largely due to an older average age and the likelihood that many had been trying to conceive unsuccessfully before seeking fertility treatment.
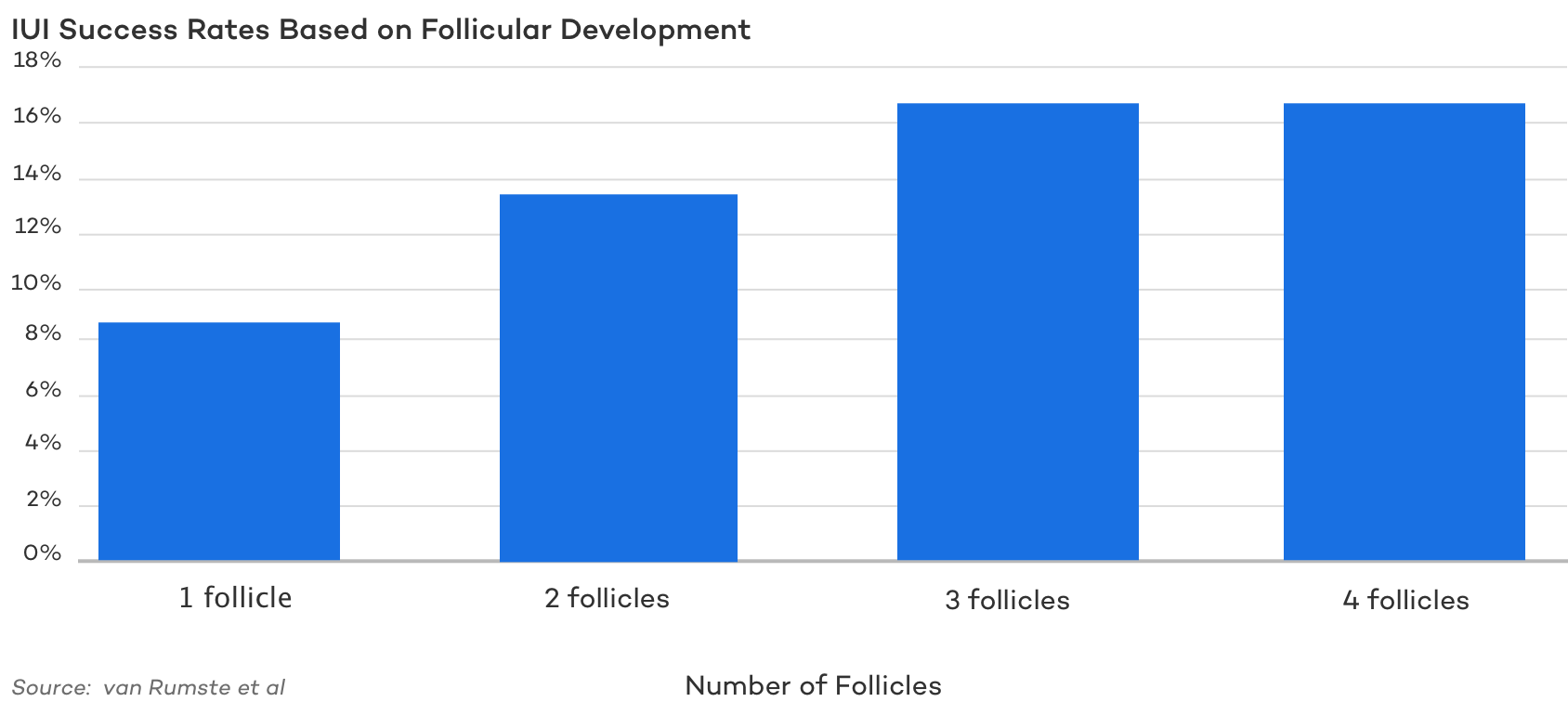
IUI Success Rate By the Number of Follicles
The goal of ovarian stimulation with fertility medications is to produce multiple follicles, which means more eggs are available for fertilization and, in turn, a higher chance of conception in that cycle.
In short, more follicles generally increase the odds of success, up to a point. The challenge is finding the balance: enough eggs to boost chances of pregnancy, but not so many that it results in twins, triplets, or even higher-order multiples.
Singleton pregnancies carry much lower risks for both mother and baby, which is why most doctors and fertility clinics aim for a single healthy pregnancy. For this reason, most practices will not proceed with IUI if a woman develops four or more mature follicles in a medicated cycle.
Research confirms that multi-follicular development is associated with higher pregnancy rates in IUI cycles with controlled ovarian hyperstimulation (COH). However, the same studies also show a higher risk of multiple gestations with increasing follicle numbers.
IUI Success Rate By Drug Type
Most, but not all, IUI cycles are paired with fertility medications to stimulate the follicles to produce additional eggs.
Your fertility specialist will recommend medications based on your medical history, diagnosis, and preferences. The choice of medication, as well as the dosage, can significantly impact IUI success rates.
The three main medications used in medicated IUI cycles are:
- Clomid
- Letrozole
- Gonadotropins
Clomid is now used less frequently at many clinics, including CNY Fertility. Clomid and Letrozole are oral medications that signal the brain to send stronger cues to the ovaries to ovulate.
Gonadotropins are injectable medications that directly stimulate the ovaries to produce multiple follicles.
All these medications have the ultimate goal of maximizing the number of eggs available for fertilization while minimizing the risk of multiple pregnancies.
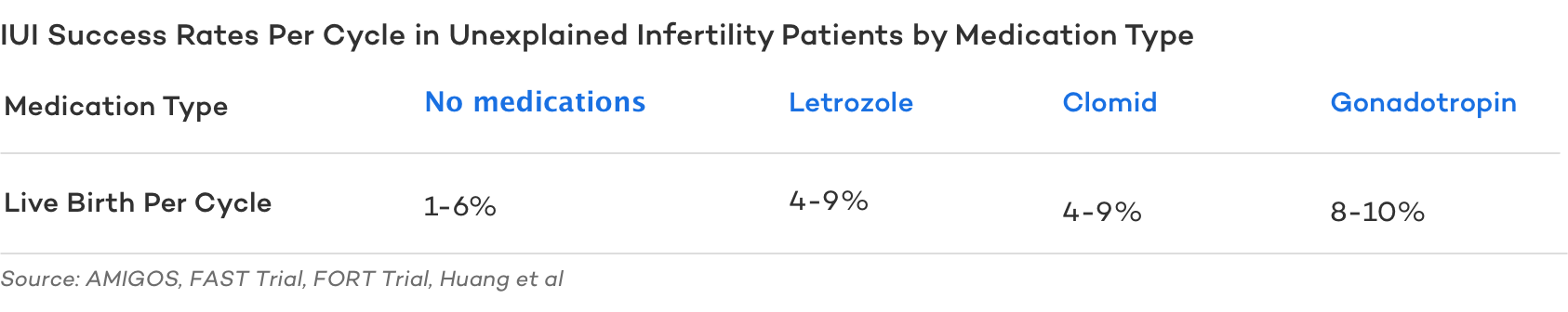
It’s important to note that although Clomid and Letrozole have similar odds of producing a live birth, letrozole generally has fewer side effects and, more importantly, produces more singleton births.
IUI Success Rate Comparing Fresh vs. Frozen Sperm
Both fresh and frozen sperm can be used successfully for IUI, but fresh sperm is generally preferred when available.
This is partly because some sperm are lost during the thawing process, and also because timing becomes more critical with washed and thawed sperm.
Washed fresh sperm typically survive 24–36 hours, while washed thawed sperm have a shorter lifespan of about 12–24 hours. The longer survival time of fresh sperm may improve the chances of conception.
One study compared pregnancy rates using fresh versus cryopreserved sperm for IUI :
- After a single cycle, pregnancy rates were higher with fresh sperm than with frozen (21.2% vs. 15.8%).
- The difference widened over three cycles (48% fresh vs. 22% frozen)
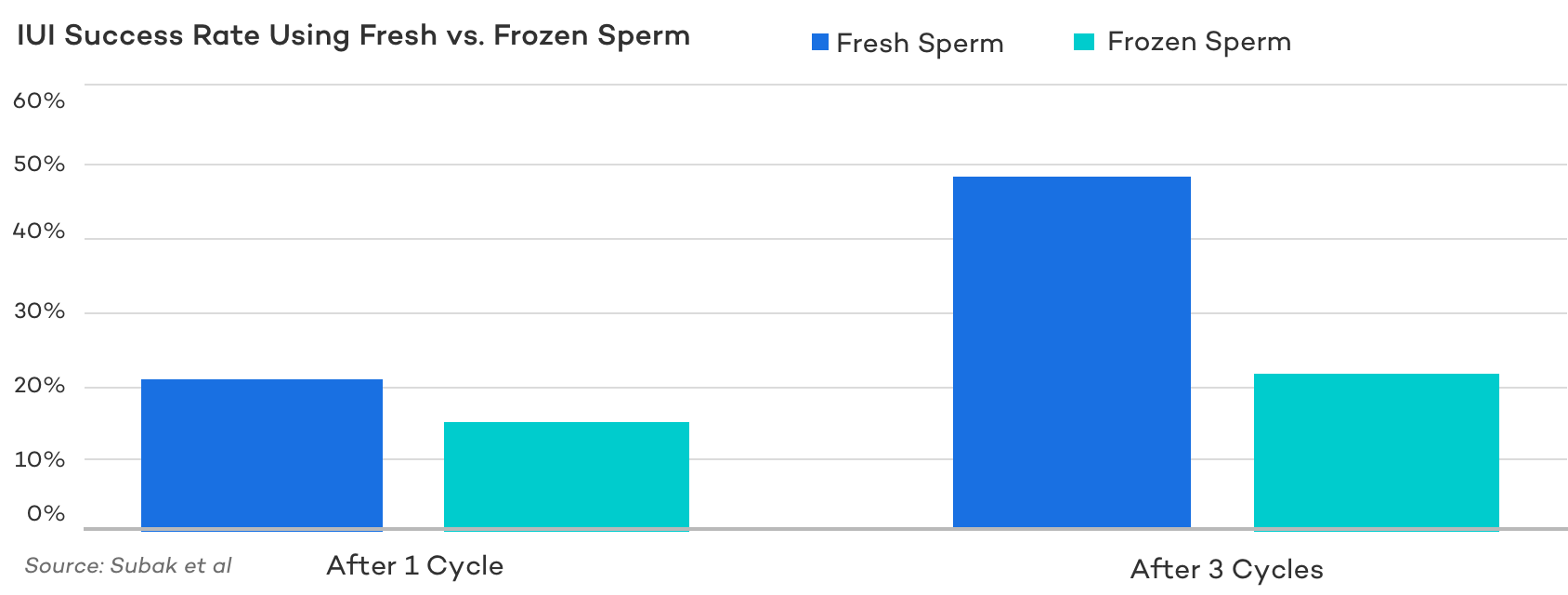
Fresh sperm isn’t always an option, especially for LGBTQ couples, single women, individuals facing severe male factor infertility, or partners who are on active duty or otherwise unable to attend fertility appointments and therefore rely on donor sperm.
Many fertility specialists emphasize that the timing of the IUI and an adequate concentration of sperm, measured as the total motile count (TMC), are the factors that most strongly influence success.
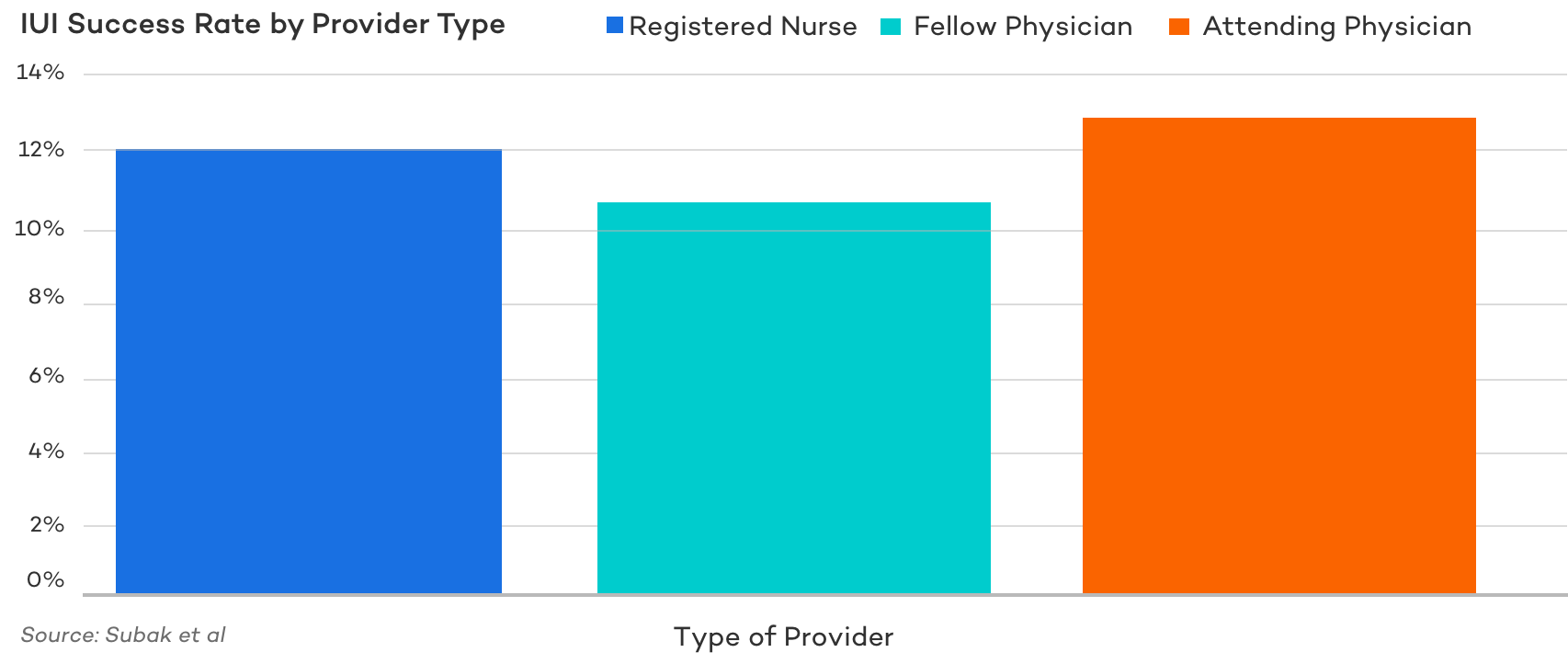
IUI Success Based on Provider Type
In recent years, nurse practitioners and registered nurses have begun performing a growing number of IUI procedures. You might wonder if IUI success rates vary depending on whether a nurse or a doctor performs the insemination.
A study comparing the outcomes of IUIs performed by registered nurses, attending physicians, and fellowship-trained physicians found no significant difference in pregnancy or live birth rates, regardless of who performed the insemination.
While many factors can influence IUI success, provider type does not appear to be one of them.
IUI Success Rates after Multiple Cycles
With natural conception, success is often measured over many months of trying, typically 6 to 12 months.
That’s why fertility specialists recommend couples under age 35 try on their own for a year before seeking help, while couples over 35 are advised to try for only 6 months.
Age plays a major role, and earlier intervention can be especially important for women over 35.
The same principle of repetition applies to IUI, but only up to a point. Research shows that the vast majority of IUI pregnancies occur within the first three to four treatment cycles.
One study found that 88% of successful IUIs happened within three cycles and 95% within four.
Another analysis of more than 3,000 cycles found that 90% of IUI pregnancies occur within the first three attempts.
Knowing when to move on to other treatments is important for both emotional and financial well-being.
If pregnancy hasn’t been achieved after three to four IUIs, success rates tend to plateau. At that point, the cost per live birth rises sharply, making IVF the more effective and cost-efficient treatment option.
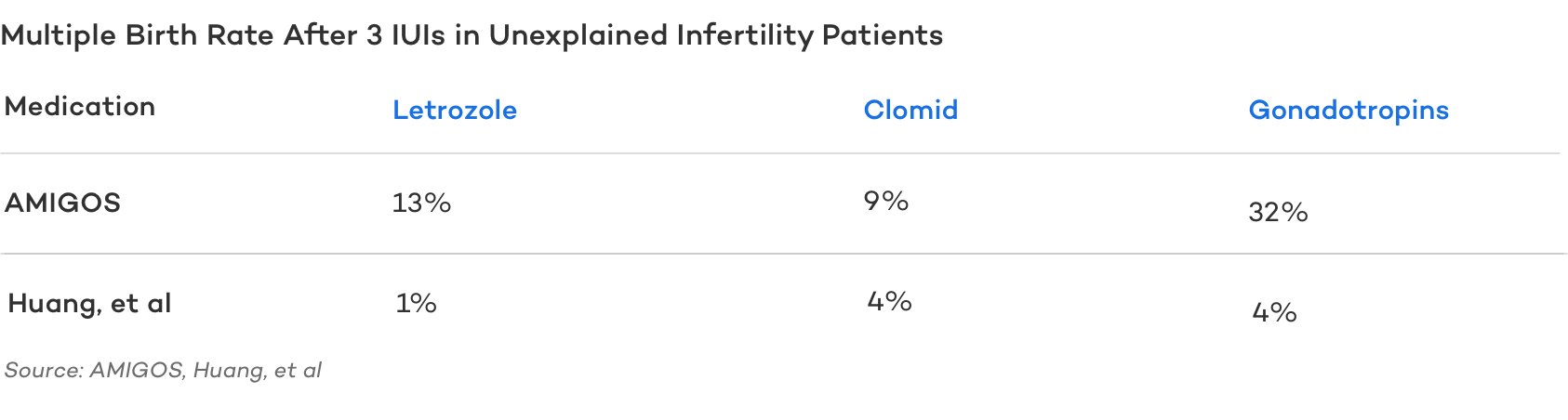
Considering Risk of Multiples as a Measure of IUI Success
IUI paired with fertility medication carries a significant risk of multiple pregnancies.
A good fertility clinic will closely monitor follicle development, adjust medications as needed, and even cancel an IUI cycle if four or more follicles are growing.
Still, the risk cannot be eliminated entirely. Unlike IVF, where patients and doctors can choose how many embryos to transfer (usually one, occasionally two), IUI offers no such control, which makes multiples more likely.
Ovarian stimulation is used with IUI to increase the number of eggs available for fertilization, which raises pregnancy chances but also increases the risk of twins or higher-order multiples.
For example, Clomid treatment carries about a 10% chance of twins and less than a one percent chance of triplets.
In contrast, gonadotropins used with IUI can lead to multiple pregnancy rates as high as 30%.
The exact risk varies between studies, largely due to the use of different dosages and protocols.
Overall, while the chance of multiples per pregnancy can range from eight percent to thirty percent depending on the medication, the risk per cycle is much lower. Only about one-half of one percent to two and a half percent of all IUI cycles actually result in multiple births.
How to Improve IUI Success Rates
Timing, egg quality, and sperm quality all play critical roles in IUI success. Medicated cycles can significantly increase the number of eggs released, which often boosts the odds of conception.
Most fertility specialists also recommend lying flat on your back immediately after the insemination. Research shows that women who remained lying down for fifteen minutes after IUI were about ten percent more likely to conceive compared to those who got up right away.
Beyond the procedure itself, lifestyle changes are among the most effective ways to support your overall health and enhance your chances of success.
At CNY Fertility, we recommend the following steps to improve fertility prior to beginning an IUI cycle:
- Eat fertility superfoods and a high-fat, low-carb fertility diet to give your body all the nutrients it needs, reduce inflammation, and improve hormone function.
- Take male and female fertility supplements to help enhance egg quality, sperm quality, improve implantation, and ultimately increase your odds of IUI success. Many nutrients you’ll find in fertility supplements including CoQ10/ubiquinol, inositol, Vitamin D, and more have been extensively studied and clinically shown to increase IUI success rates. Here at CNY Fertility, we recommend Molecular Fertility’s line of science-backed supplements for men and women.
- Limit high-intensity exercise which can cause heat and inflammation and take away blood flow from your core. Instead focus on yoga, Tai Chi, light weights and stretching, or walking with a friend.
- Certain prescription medications can go a step further than diet and lifestyle changes in reducing inflammation and supporting fertility. For patients diagnosed with conditions like PCOS or endometriosis, several medications can help balance hormones and improve reproductive health. In cases of an overactive immune system, treatments such as low-dose naltrexone (LDN), intravenous immunoglobulin (IVIG), or tacrolimus may be used to modulate immune activity. Since infertility is often linked to underlying health conditions, treating these issues directly can meaningfully improve the chances of conception. .
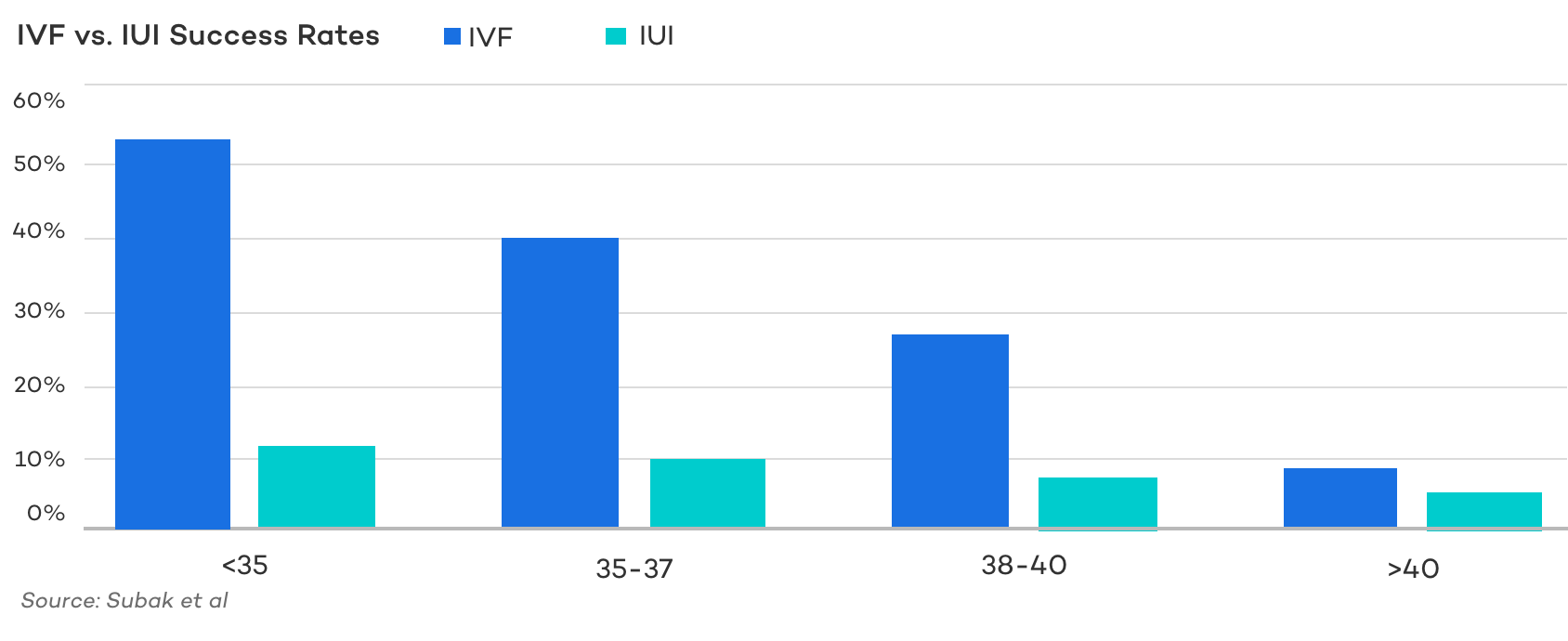
IVF vs. IUI Success Rates
When it comes to comparing fertility treatments, the discussion of IUI versus IVF is one of the most common.
Statistically, there is little debate: In Vitro Fertilization (IVF) consistently provides higher success rates and typically leads to pregnancy more quickly than IUI, regardless of age or diagnosis.
Over the past two decades, IVF techniques have advanced dramatically, while IUI success rates have remained relatively stable.
However, the greater effectiveness of IVF comes with added costs. Both physical and financial. IVF is more involved, requiring multiple medications and surgical procedures, and it is significantly more expensive.
While repeated IUI cycles can sometimes approach the cumulative success rates of IVF, on a per-cycle basis, IUI remains much less effective.
Rate of Multiples with IUI vs. IVF
For comparison purposes, how does the multiple birth rate for IVF compare to IUI?
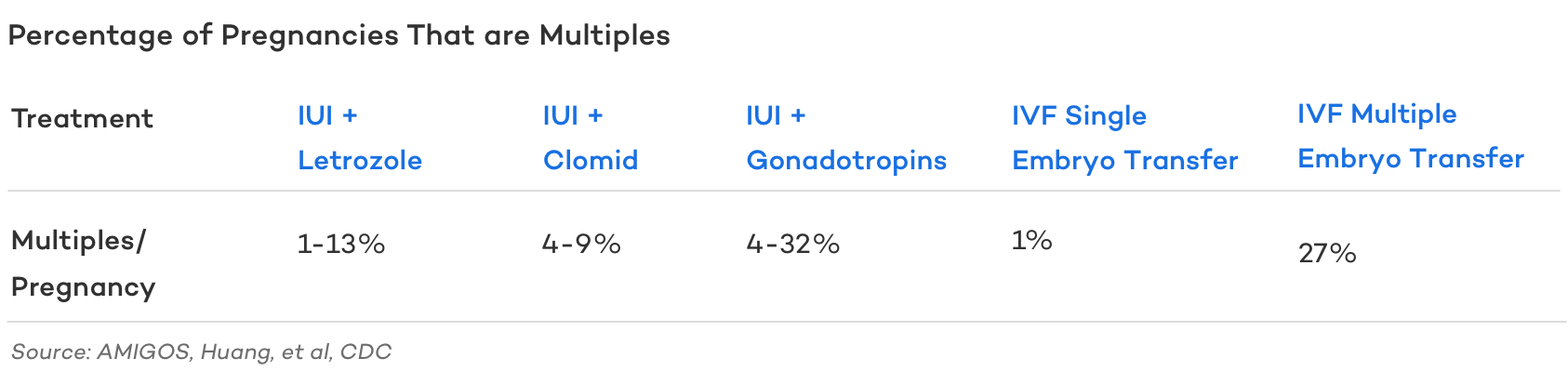
According to a large study of nearly one million single embryo transfers, the chance of a twin or multiple birth due to zygotic splitting after transferring a single embryo is only 1.6%.
Another study comparing patients who had one blastocyst transferred versus two found no difference in live birth rates, no incidence of twins in the single transfer group, and a twin birth rate of 29.02% in the double blastocyst group.
In the early days of IVF, doctors transferred multiple embryos to improve the odds of implantation. Today, advanced techniques allow embryologists to better assess embryo quality, making it safer to aim for one healthy baby at a time.
The American Society for Reproductive Medicine (ASRM) recommends single embryo transfer (eSET) for patients under 38 and for all PGT euploid embryos. eSET lowers the risk of multiples while maintaining nearly the same pregnancy rates. Because fewer embryos are transferred per cycle, multiple births with IVF are now far less common. Electively transferring more than one embryo is what raises the risk to levels similar to IUI.
IUI Success Stories
When you’re trying to conceive, few things inspire more hope than hearing real IUI success stories from others who faced similar challenges and went on to build their families.
While IUI may not always work on the first attempt and sometimes requires patience or adjustments in protocol, it can and does lead to pregnancy. The success stories speak for themselves.
- Read about how Danielle and Joseph overcame PCOS by adopting a keto diet and doing medicated IUI.
- Learn how Candice and Patrick incorporated acupuncture, Maya massage, and keto along with IUI and Letrozole to welcome their rainbow baby.
- Cristine and Mervin used medicated IUI to beat male factor infertility and welcome their son, Mervy.
- Ramona and Stepan combined conceived their oldest son Zayn with IUI. Ramona switched to keto and was able to conceive their younger son Iden naturally.
- Christine and Sam switched to IUI with injectables for their second IUI cycle and successfully conceived triplets- Viola, John Henry, and Vivienne.
Bottom Line
Intrauterine insemination (IUI), also known as artificial insemination, is one of the least invasive fertility treatments and can be highly effective in the right circumstances.
It is often a good first-line option for many women and couples, particularly those with mild male factor infertility, ovulatory dysfunction, unexplained infertility, or for single women and same-sex couples.
Success depends on many factors, with age, diagnosis, and the medication protocol playing the most significant roles.